Short Summary
Written by Dr. Peter Attia, Outlive covers all elements of longevity, from exercise and nutrition to sleep and emotional health. Attia also takes a close look at what he calls ‘The Four Horsemen’ of aging: metabolic dysfunction, heart disease, cancer, and neurodegenerative diseases like Alzheimer’s. All four chronic diseases — which kill almost everyone in some form — are discussed at length, including the factors driving each of them.
Key Takeaways



Favorite Quote
“Which brings us to perhaps the most important difference between Medicine 2.0 and Medicine 3.0. In Medicine 2.0, you are a passenger on the ship, being carried along somewhat passively. Medicine 3.0 demands much more from you, the patient: You must be well-informed, medically literate to a reasonable degree, clear-eyed about your goals, and cognizant of the true nature of risk. You must be willing to change ingrained habits, accept new challenges, and venture outside of your comfort zone if necessary. You are always participating, never passive. You confront problems, even uncomfortable or scary ones, rather than ignoring them until it’s too late. You have skin in the game, in a very literal sense. And you make important decisions.”
Book Notes 
Introduction
- Peter Attia, MD — Peter Attia is the author of this book. He received his medical degree from Stanford University School of Medicine and trained at Johns Hopkins Hospital in general surgery. He also trained at the NIH as a surgical oncology fellow at the National Cancer Institute, where his research focused on immune-based therapies for melanoma.
- ‘Catching Eggs’ — Attia starts the book reflecting on his early days in the medical profession. While training at Johns Hopkins, he often had a dream where he was on a random street next to a tall building and was tasked with catching eggs that were being launched from the top of the building before they splattered. The eggs were an analogy for patients’ health problems and catching them was an analogy for saving the patients. Inevitably, he couldn’t catch every egg and save every patient. That reality was a sad one and led him to leave the medical profession for a short period. What made him return was a renewed mindset on health and medicine. Rather than catching the eggs, Attia returned to medicine with a different approach: take out the guy at the top of the building throwing them. In other words, Attia wanted to focus on preventing health problems, and that’s what this book is about.
- Interesting Fact — Pancreatic cancer grows silently, without symptoms, and by the time it is discovered, it is often quite advanced. Surgeons often opt for the Whipple Procedure to combat the cancer. This involves removing the head of the patient’s pancreas and upper part of the small intestine called the duodenum. It’s a difficult, dangerous operation, and in the early days it was almost always fatal. Today, 99% of patients survive the procedure.
Ch. 1: The Long Game
- Longevity — Attia’s focus as a physician is now on longevity. He’s focused on helping people live longer, healthier lives by preventing some of the chronic diseases that kill people. Longevity isn’t just about living longer; it’s about the quality of your years. You want to live a life free of disability and disease. Through his work, Attia helps people maintain and improve mental function as they age. The key is to start preventative measures and habits as soon as possible. That’s what this book will discuss.
- Quote (P. 11): “Already, in midlife, the warning signs abound. I’ve been to funerals for friends from high school, reflecting the steep rise in mortality risk that begins in middle age. At the same time, many of us in our 30s, 40s, and 50s are watching our parents disappear down the road to physical disability, dementia, or long-term disease. This is always sad to see, and it reinforces one of my core principles, which is that the only way to create a better future for yourself — to set yourself on a better trajectory – is to start thinking about it and taking action now.”
- The ‘Four Horsemen’ & Slow Death — In 1900, life expectancy was in the 40s, and most people died from “fast” causes like accidents, infectious diseases, and injuries. Today, life expectancy is in the 70s and 80s, and “slow death” kills most people. Attia refers to the chronic diseases of “slow death” as the ‘Four Horsemen.’ These diseases often begin to establish themselves in the body years before they are detected. To achieve longevity, it’s important to understand and confront them as early as possible. The ‘Four Horsemen’ include:
- Heart Disease
- Cancer
- Neurodegenerative Disease
- Type 2 Diabetes / Related Metabolic Dysfunctions
- Medical Training — One of the challenges with longevity is that the skills and training many medical professionals develop have proven to be far more effective in combating fast death than slow death. Doctors have an amazing ability to heal broken bodies after severe trauma, but the ‘Four Horsemen’ have been harder to solve. Although mortality rates related to cardiovascular disease have been cut by two-thirds in the last 60 years, death rates from cancer have hardly budged in the over 50 years since the War on Cancer was declared.
- Proactive, Not Reactive — The key to longevity is prevention. With many of the chronic ‘Four Horsemen’ diseases, by the time medical intervention occurs, it’s too late — the disease has already taken hold and there’s not a lot a doctor can do. Prevention and a proactive (rather than reactive) mindset are the keys. For example, no medical treatment for late-stage lung cancer has reduced mortality rates as much as the worldwide reduction in smoking that has occurred over the past 20 years. Taking preventative measures is one of the best ways to improve our chances at living longer, healthier lives.
- Quote (P. 13): “While the prevalence of each of the Horsemen diseases increases sharply with age, they typically begin much earlier than we recognize, and they generally take a very long time to kill you. Even with someone who dies ‘suddenly’ of a heart attack, the disease had likely been progressing in their coronary arteries for two decades. Slow death moves even more slowly than we realize. The logical conclusion is that we need to step in sooner to try to stop the Horsemen in their tracks — or better yet, prevent them all together.”
- Quote (P. 14): “I believe that our goal should be to act as early as possible, to try to prevent people from developing Type 2 diabetes and all the other Horsemen. We should be proactive instead of reactive in our approach. Changing that mindset must be our first step in attacking slow death. We want to delay or prevent these conditions so that we can live longer without disease, rather than lingering with disease. That means that the best time to intervene is before the eggs start falling.”
- Takeaway — Rather than waiting for a health problem to pop up and then reacting to it, we have to be proactive by taking preventive measures as early as possible. The mindset here is really important. Having a proactive, preventative mindset is half the battle.
- Interesting Fact — Epinephrine is adrenaline. It’s both a neurotransmitter and a hormone, but it acts mainly as a hormone. Epinephrine, also known as adrenaline, plays an important role in your body’s fight-or-flight response. It’s also given to hospital patients as a medication in many life-threatening situations.
- Attia’s Studies — Attia didn’t begin studying longevity seriously until the age of 36. Although he was an accomplished surgeon, exercised regularly, and maintained a fairly healthy diet, he was 215 pounds and had a family history of heart disease. These factors inspired him to study the scientific literature on nutrition and metabolism, heart disease, cancer, neurodegenerative diseases, and gerontology — which is the effort to understand what drives the aging process and how it can be slowed. A few of his key findings, each of which will be described in more detail in this book, include:
- Cholesterol Panel — The typical cholesterol panel that you receive and discuss at your annual physical, along with many of the underlying assumptions behind it (e.g. “good” and “bad” cholesterol), is misleading and oversimplified to the point of uselessness. It doesn’t tell you nearly enough about your actual risk of dying from heart disease.
- Metabolic Health — The same metabolic issues that lead to Type 2 diabetes can also contribute to heart disease, cancer, and Alzheimer’s disease. By addressing your metabolic health, your can lower the risk of each of these diseases.
- Protein — Protein, more than carbs and fat, is the most important macronutrient and becomes critically important as we age.
- Exercise — Exercise is by far the most important longevity “drug.” No other habit does nearly as much to prolong your lifespan and preserve your cognitive and physical functions.
- Quote (P. 16): “Perhaps my biggest takeaway (from his studies) was that modern medicine does not really have a handle on when and how to treat the chronic diseases of aging that will likely kill most of us. This is in part because each of the Horsemen is intricately complex, more of a disease process than an acute illness like a common cold. The surprise is that this is actually good news for us, in a way. Each one of the Horsemen is cumulative, the product of multiple risk factors adding up and compounding over time. Many of these same individual risk factors, it turns out, are relatively easy to reduce or even eliminate. Even better, they share certain features or drivers in common that make them vulnerable to some of the same tactics and behavioral changes we will discuss in this book. Medicine’s biggest failing is in attempting to treat all of these conditions at the wrong end of the timescale — after they are entrenched — rather than before they take root.”
- Takeaway — By developing good habits, you can lower your chances of encountering heart disease, diabetes, cancer, and neurodegenerative diseases because these diseases possess some of the same, or similar, risk factors.
- Chapter Takeaway — Half of the longevity battle is your mindset. It’s critical to adopt a proactive, preventative mindset when it comes to your health. Most people have a reactionary mindset — we wait until something pops up to begin addressing it. The problem is that many chronic diseases entrench themselves in your body far before they are detected. By the time they are detected, it can be an uphill battle to cure them. Establishing a set of good habits can help you live longer and improve the quality of your years.
Ch. 2: Medicine 3.0
- Eras of Medical History — There have been two distinct eras of medical history, and we may be on the verge of a third. In their own ways, each of the eras helped advance the medical profession to what it is today. Attia refers to these eras as Medicine 1.0 and Medicine 2.0. He also explains that we may be crossing into the beginnings of Medicine 3.0.
- Medicine 1.0 — This era was marked by Hippocrates, an Ancient Greek physician who is known as one of the most important figures in the history of medicine. The Hippocratic Oath — which is an oath physicians take “to do no harm” to patients — is attributed to Hippocrates. In this era, conclusions were largely reached using observation and guesswork, some of which was on target and some of which wasn’t. The physicians of this time period simply didn’t have access to the tools, resources, and scientific information available to us now to reach accurate conclusions. Although much of Medicine 1.0 missed the mark, Hippocrates’s major contribution was the insight that diseases are caused by nature and not by actions of the gods, as had previously been believed. This was a big step in the right direction.
- Medicine 2.0 — Medicine 2.0 arrived in the mid-19th century with the advent of the germ theory of disease, which replaced the previously-held idea that most illnesses were spread by bad air. This led to improved sanitary practices by physicians and the development of antibiotics. In 1865, Joseph Lister first demonstrated the principle of antiseptic surgery, using sterile techniques to operate on a patient. It was the first application of the germ theory of disease. Prior to this era, germs had not been discovered. Also in this era (1628), Sir Francis Bacon presented the scientific method and hypothesis testing which completely changed the way we think about science. Penicillin, a medication used to manage and treat a wide range of infections, was also a game-changing discovery in this era. Other milestones in this era include successes in containing HIV and AIDS, polio, smallpox, hepatitis C, and COVID-19.
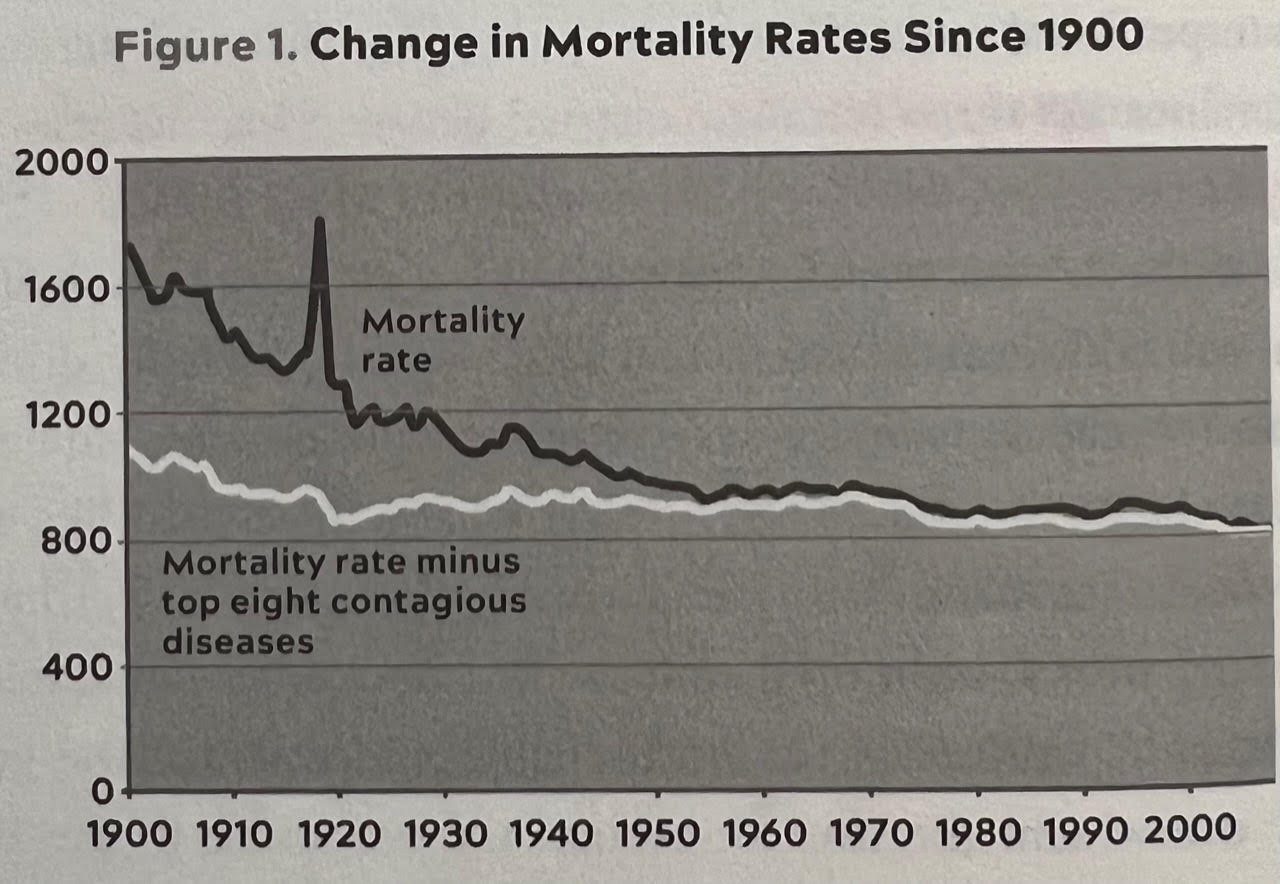
- Medicine 2.0 & Mortality Rates — Although the Medicine 2.0 era has been highly successful, we haven’t made great progress against long-term diseases like cancer and the other Horsemen. Lifespans have nearly doubled since the late 1800s, but the majority of that progress may have resulted from antibiotics and improved sanitation. These alone have helped significantly reduce the number of deaths from contagious bacterial diseases. In fact, if you look at mortality rates since the year 1900 and subtract out deaths from the eight top infectious diseases (which have been controlled by antibiotics), overall mortality rates declined relatively little over the course of the 20th century. See chart below.
- Toward Medicine 3.0 — Chronic diseases (the Four Horsemen) start as minor risk factors that build over years and decades until a terrible event happens, which is why Attia believes a new way of thinking about these chronic diseases, their treatment, and how to maintain long-term health is needed. He calls a proactive, preventative approach to these diseases ‘Medicine 3.0.’ The goal with this approach is to prevent the diseases from building up over time through good habits and proactive detection strategies. These habits, paired with the incredible technology capabilities currently available (and those still in development) that are going to help doctors deliver truly personalized treatment, are the characteristics of Medicine 3.0.
- Quote (P. 29): “The banks’ problem was not all that different from the situation faced by some of my patients: their seemingly minor risk factors had, over time, compounded into an unstoppable, asymmetric catastrophe. Chronic diseases work in a similar fashion, building over years and decades — and once they become entrenched, it’s hard to make them go away. Atherosclerosis, for example, begins many decades before the person has a coronary ‘event’ that could result in their death. But that event, often a heart attack, too often marks the point where treatment begins.”
- Quote (P. 29): “The goal of this new medicine — which I call Medicine 3.0 — is not to patch people up and get them out the door, removing their tumors and hoping for the best, but rather to prevent the tumors from appearing and spreading in the first place. Or to avoid that first heart attack. Or to divert someone from the path to Alzheimer’s disease.”
- Characteristics of Medicine 3.0 — More so than the great technology that is already available and the other pieces of technology coming in the next few years and decades, Medicine 3.0 is about mindset and shifting the way we approach health. Again, the key is a mindset of proactive prevention. Attia presents four main points in his Medicine 3.0 model:
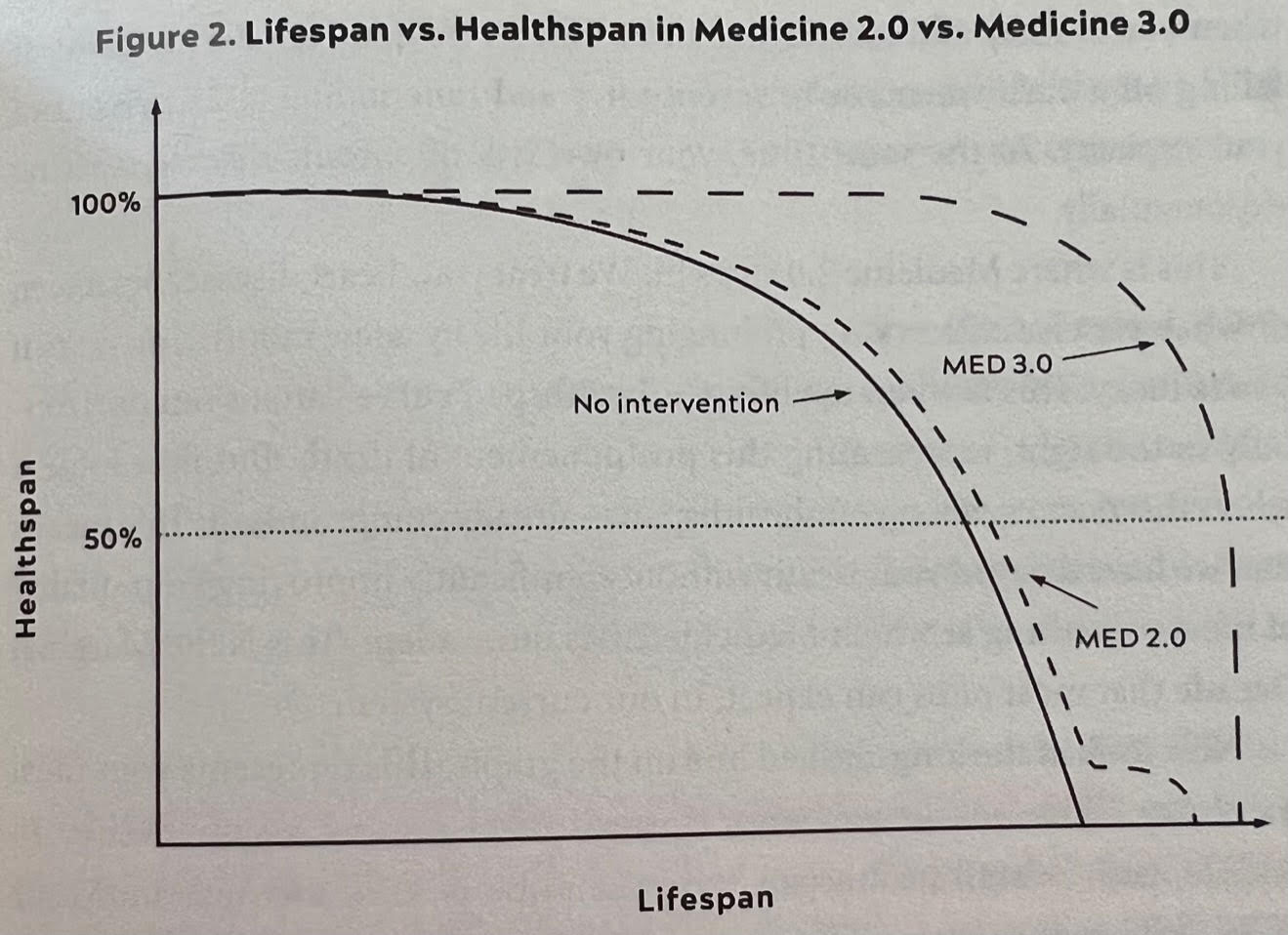
- Prevention — Medicine 3.0 is all about adopting an approach of prevention. The emphasis is on prevention more than treatment. Medicine 2.0 is reactionary and tries to figure out how to fix the problem; Medicine 3.0 is proactive and is focused on preventing the problem altogether. Put another way, Medicine 2.0 is focused on helping us live longer with disease, while Medicine 3.0 is about delaying or preventing disease altogether through preventative measures.
- Personalized Planning — Medicine 2.0 uses the findings of clinical trials and evidence-based testing to create “average benchmarks” and then uses those “average benchmarks” for everyone. The problem is that everyone is different. Just because a patient’s test results are hitting the “average” benchmarks reported in a clinical or evidence-based study does not mean they are in optimal health. Medicine 3.0 takes a patient’s data and determines how he/she is similar or different than the “average” subject in these studies, and how the findings may or may not be applicable to them. Decisions are then made about a patient’s health plan and medical treatment.
- Understanding and Accepting Risk — In Medicine 3.0, our starting point is the honest assessment, and acceptance, of risk — including the risk of doing nothing. You have to be willing to ask deeper questions about risk vs. reward. When results of various clinical studies come out advocating for or against a certain treatment or therapy, you can’t just accept the results without asking deeper questions about the study’s possible limitations and biases. The reality is that we are all different and one course of action that isn’t right for one person may be the right one for another person. There has to be some willingness to take risks. It doesn’t mean you have to take risks left and right, but you have to be willing to at least have a conversation.
- Healthspan — Medicine 3.0 is focused not just on lifespan, but also healthspan, or the overall quality of your years. You want more out of life than simply the absence of sickness or disability. Ideally, you want to be thriving, in every way, throughout the latter half of your life. Medicine 2.0 largely ignores the factors that go into healthspan (e.g. exercise, nutrition, sleep) and focuses more on treating problems that come up.
- Interesting Fact — Before the Titanic hit an iceberg and sank in the Atlantic Ocean in 1912, the massive steamship received an urgent message from another vessel that it was headed for an icefield. The message was ignored. An hour later, the ship received another urgent telegraph message from a different ship. It was ignored. Forty-five minutes after the last message, the ship’s lookout spotted the fatal iceberg 500 yards away. It was too late.
- “I’m the Captain Now” — One of the biggest themes of this book is that you are not a passive bystander on your health ship. You are the captain. This is the mindset you need to have. You have to take accountability for forming good habits that will help prevent the ‘Four Horsemen.’ This means exercising, eating well, reading medical reports, asking your doctor difficult questions, taking risks, confronting scary problems, and more.
- Quote (P. 35): “Which brings us to perhaps the most important difference between Medicine 2.0 and Medicine 3.0. In Medicine 2.0, you are a passenger on the ship, being carried along somewhat passively. Medicine 3.0 demands much more from you, the patient: You must be well-informed, medically literate to a reasonable degree, clear-eyed about your goals, and cognizant of the true nature of risk. You must be willing to change ingrained habits, accept new challenges, and venture outside of your comfort zone if necessary. You are always participating, never passive. You confront problems, even uncomfortable or scary ones, rather than ignoring them until it’s too late. You have skin in the game, in a very literal sense. And you make important decisions.”
- Chapter Takeaway — Medicine 3.0, as Attia presents it, is all about prevention and proactive detection strategies. Whereas Medicine 2.0 expects patients to be passive bystanders on their health journey, Medicine 3.0 requires patients to take more of a leadership role. It’s about being proactive rather than reactive. This requires a fundamental shift in thinking because most people have been trained to react to health problems that pop up (catching the eggs) rather than preventing them (taking out the egg thrower).
Ch. 3: Objective, Strategy, Tactics
- Dying in Slow Motion — For most people today, the aging process typically involves living pretty comfortably until around age 50. In midlife, we gradually begin to experience changes and a decline in physical and cognitive abilities. Around age 70 or 75, the decline steepens and modern medicine steps in to prolong your life for a few more months or years. But your last decade or so really stinks. You’re basically just holding on and dying in slow motion. Alternatively, what you want to achieve is a life where you are getting stronger, both mentally and physically, over time. You want to be thriving in your 50s, 60s, and 70s. In this scenario, we live longer and better for longer. We’re delaying death. Our decline will be steep, but relatively brief. Both of these aging processes are summarized in the chart below.
- Quote (P. 40): “Now look at the long-dashed line on the graph. This represents your ideal trajectory. This is what you want. Instead of beginning a slow decline in midlife, your overall healthspan stays the same or even improves into your 50s and beyond. You’ll be fitter and healthier at 55 and even 65 than you were at 45 and will remain physically fit and cognitively sharp well in your 70s and 80s, and possibly beyond. You will seem like someone a decade younger than the age on your passport, and possibly two… Instead of a lousy Marginal Decade, we get to enjoy what feels more like a Bonus Decade — or decades — when we are thriving in every dimension. This is our objective: to delay death, and to get the most out of our extra years. The rest of our lives becomes a time to relish rather than to dread.”
- Aging & the ‘Four Horsemen’ — Aging is the common risk factor among the Four Horsemen. As you grow older, the risk grows that one of these diseases has begun to take hold in your body. The disease will normally take years or decades to develop before it strikes. This is why you have to have an overall preventative strategy and set of tactics in place to combat these diseases. Otherwise, the pull of life’s gravity will take you down quickly as you get older.
- Quote (P. 43): “The very process of aging itself is what makes us vulnerable to these diseases, while also affecting our healthspan. Someone who drops dead of a heart attack did not just get sick an hour earlier. The disease was working inside them, silently and invisibly, for decades. As they grew older, their own internal defense mechanisms weakened, and disease gained the upper hand.”
- Components of Healthspan & Deterioration — There are three primary components of healthspan, which is essentially the overall quality of your health throughout your life. As the chart above describes, our goal is to extend healthspan as far out as possible. Ideally, we want to feel good for as long a humanly possible. The components of healthspan decline are below. Our goal is to minimize these, defying or avoiding all of these vectors of decline simultaneously.
- Cognitive Decline — Your processing speed slows down and you can’t solve complex problems with the quickness and ease that you used to. Your memory fades. You just aren’t as sharp.
- Physical Decline — This might precede or follow cognitive decline. Frailty begins to get you. You lose muscle mass and strength, along with bone density, stamina, stability, and balance. Your aerobic fitness declines. Eventually bringing in the groceries is almost impossible.
- Emotional Decline — Unlike the others, this one doesn’t necessarily have to do with age, but it’s just as important as physical and cognitive health. Having strong emotional health is critical to longevity.
- Quote (P. 47): “The important distinction here is that while actual death is inevitable, this deterioration they we’re talking about is less so. Not everyone who dies in their 80s or 90s passes through the valleys of cognitive, physical, or emotional destruction on the way there. They are preventable — and I believe that they are largely optional, despite their ever-increasing gravitational pull over time.”
- Longevity Tactics — Medicine 2.0 relies on two types of tactics: procedures (e.g. surgery) and medications. Our tactics in Medicine 3.0 fall under five broad domains, each of which will be discussed at length in the book. These tactics are critical to a preventative and proactive longevity strategy. We have to chip away at these and maximize them to the best of our abilities. They are:
- Exercise — This involves a variety of training. We need to build our physical fitness to a level that will allow for longevity. Strength, stability, aerobic efficiency, and peak aerobic capacity are the five pillars of exercise. Increasing your limits in each of these areas is necessary to maximize lifespan and healthspan.
- Quote (P. 48): “This is another area where my thinking has changed over time. I used to prioritize nutrition over everything else, but I now consider exercise to be the most potent longevity ‘drug’ in our arsenal, in terms of lifespan and healthspan. The data are unambiguous: exercise not only delays actual death but also prevents both cognitive and physical decline better than any other intervention. We also tend to feel better when we exercise, so it probably has some harder-to-measure effect on emotional health as well.”
- Nutrition — The best science out there says that what you eat matters, but the first order of business is how much you eat. How many calories you take into your body is critical.
- Sleep — Sleep has been ignored by too many for too long. Sleep is absolutely critical to so many things that go on inside your body. A lot of bad things happen when sleep is compromised.
- Emotional Health — This is just as important as the other tactics. You have to make sure you are keeping your emotional house in order. You want to live a longer and healthier life, but you also want to do it while being happy.
- Exogenous Molecules — These are things like pharmaceutical drugs, hormones, or supplements. These molecules, including lipid-lowering medications, are important to our longevity.
- Exercise — This involves a variety of training. We need to build our physical fitness to a level that will allow for longevity. Strength, stability, aerobic efficiency, and peak aerobic capacity are the five pillars of exercise. Increasing your limits in each of these areas is necessary to maximize lifespan and healthspan.
- Chapter Takeaway — Your goal should be to get stronger, mentally, physically, and emotionally, over time. The typical person experiences physical and cognitive challenges in their midlife years and it’s a slow descent from there. Modern medicine can help prolong life to a certain degree at the end, but the person is usually not comfortable in their final years. Your aim should be to extend your healthspan as far out as possible through good habits and preventative tactics. The goal is to delay aging and the Four Horsemen for as long as possible. When you do decline, it will be brief; you won’t be lingering in discomfort for very long. A few lifestyle changes can help you get stronger into your 50s, 60s, and 70s.
Ch. 4: Centenarians
- Interesting Fact — Frenchwoman Jean Calment lived to be 122 years old, making her the oldest person to have ever lived. She lived from 1875-1997.
- Centenarians — Centenarians are people who live to be 100 years old or older. It’s an elite class — in 2021, there were under 100,000 centenarians in the U.S. Centenarians make up just 0.03% of the population, or 1 out of every 3,333 people.
- Centenarians & Genes — Various studies have shown that the older you get, the more genes start to matter. What’s remarkable about centenarians is the fact that they are able to delay chronic diseases like the Four Horsemen by 1-3 decades. There’s no doubt that centenarians were blessed with amazing genes and genes are a major reason they are able to live so long and delay these diseases. But genes aren’t the only factor in play when it comes to a person’s lifespan and healthspan. We can try to achieve a longer and lifespan and healthspan by being intentional.
- Quote (P. 65): “In mathematical terms, the centenarians’ genes have bought them a phase shift in time — that is, their entire lifespan and healthspan curve has been shifted a decade or two (or three!) to the right. Not only do they live longer, but these are people who have been healthier than their peers, and biologically younger than them, for virtually their entire lives. When they were 60, their coronary arteries were as healthy as those of 35-year-olds. At 85, they likely looked and felt and functioned as if they were in their 60s. They seemed like people a generation younger than the age on their driver’s license. This is the effect that we are seeking to mimic.”
- Quote (P. 65): “The centenarians not only live longer but live longer in a healthier state, meaning many of them get to enjoy one, or two, or even three Bonus Decades… The difference is that while most centenarians seem to get their longevity and good health almost accidentally, thanks to genes and/or good luck, the rest of us must try to achieve this intentionally.”
- Quote (P. 69): “But one individual gene, or even three dozen genes, is unlikely to be responsible for centenarians’ extreme longevity and healthspan. Broader genetic studies suggest that hundreds, if not thousands, of genes could be involved, each making their own small contribution — and that there’s no such thing as a ‘perfect’ centenarian genome. This is actually good news for those of us without centenarians in our family tree, because it suggests that even on this genetic level there may be no magic bullet; even for centenarians, longevity may be a game of inches, where relatively small interventions, with cumulative effects, could help us replicate the centenarians’ longer lifespan and healthspan. Put another way, if we want to outlive our life expectancy and live better longer, we will have to work hard and earn it — through small, incremental changes.”
- Studying Centenarians — Although we can’t replicate a centenarian’s genotype (their genes), we can take lessons from how they achieved their extreme longevity and try to mimic their phenotype, the physical traits that enable them to resist disease and survive for so long. In other words, we can identify specific genes that give centenarians their edge and try to mimic the effects of those genes. A handful of potential longevity genes have emerged in various studies of centenarians that could be relevant to our health strategy:
- APOE — This gene is related to cholesterol metabolism, glucose metabolism, and Alzheimer’s disease risk. It shuttles cholesterol around the body (especially the brain) and has three variants: e2, e3, and e4. Having one or two copies of the e4 variant seems to multiply a person’s risk of developing Alzheimer’s disease. The e2 variant, however, seems to protect against it and is highly associated with longevity. One study found people who carried at least one copy of APOE e2 (and no e4) were 30% more likely to reach extreme old age than people with the standard e3/e3 combination. Those with two copies of e4 (one from each parent) were 81% less likely to live that long. The takeaway is to test for APOE and to focus on cognitive health while paying attention to issues around cholesterol, lipoproteins, and glucose metabolism.
- CETP & APOC3 — These two cholesterol-related genes have also shown high correlation with extreme longevity and might explain why centenarians rarely die of heart disease.
- FOXO3 — This gene has been proven to be strongly associated with longevity in multiple different human ethic groups. FOXO3 regulates how other genes are expressed, meaning whether they are ‘activated’ or ‘silenced.’ Think of it like a cell’s maintenance department; it repairs cells, regulates metabolism, cares for stem cells, disposes cellular junk/waste, and does other similar things. But it doesn’t do the heavy lifting itself, like mopping, scrubbing, and minor drywall repairs. Instead, it delegates the work to other genes (its subcontractors, if you will). When FOXO3 is activated, it activates genes that keep our cells healthier. It also helps prevent cells from becoming cancerous. The takeaway is that FOXO3 can be activated or suppressed by our own behaviors. For example, when we are slightly deprived of nutrients or when we are exercising, FOXO3 tends to be more activated, which is what we want.
- Quote (P. 70): “We still have more questions than answers when it comes to the genetics behind extreme longevity, but this at least points in a more hopeful direction. While your genome is immutable, at least for the near future, gene expression can be influenced by your environment and your behaviors. For example, a 2007 study found that older people who were put on a regular exercise program shifted to a more youthful pattern of gene expression after six months. This suggests that genetics and environment both play a role in longevity and that it may be possible to implement interventions that replicate at least some of the centenarians’ good genetic luck.”
- Attack Commonalities — One of the areas where Medicine 2.0 (modern medicine) falls short is in its approach to the Four Horsemen and other diseases. Medicine 2.0 looks at these diseases as separate from each other, attacking them as if they are unrelated. In reality, there are many commonalities between these diseases, and most of them have the aging process in common. For example, the steps we take to improve metabolic health and prevent Type 2 diabetes almost certainly reduce the risk of cardiovascular disease, cancer, and Alzheimer’s simultaneously. The correct approach that needs to be taken by everybody involves both a disease-by-disease approach and a more general prevention approach:
- Disease-Specific Prevention — Forming habits and behaviors that specifically help prevent each of the individual Four Horsemen, based on what we currently know about each of them.
- General Prevention — Forming habits and behaviors that deal with all the Horsemen at onceby specifically targeting drivers and risk factors that each of them have in common.
- Chapter Takeaway — While genes are a significant reason centenarians live so long, they aren’t everything and those of us who don’t have supergenes can “make up for” an ‘average’ genetic profile through specific actions and behaviors that maximize certain genes that have proven to be associated with longevity. Both genetics and environment matter.
Ch. 5: Eat Less, Live Longer
- Interesting Fact — Easter Island in Chile is the world’s most isolated body of land that is inhabited by humans. The island’s shoreline is lined with mysterious giant stone heads, called moai 🗿. The island was named by European explorers who landed there on Easter Sunday in 1722. It’s an extremely isolated place and is only 63 square miles. The nearest human settlement is more than 1,000 miles away. This is also where a molecule named rapamycin was discovered.
- Rapamycin — This amazing molecule was discovered on Easter Island in 1964 and has completely transformed transplant medicine because of its positive effects on the immune system. Patients are given this drug when they receive a transplant of any kind because it helps their body accept their new organ. It essentially helps suppress the immune system and prevents it from attacking the foreign organ. In 2007, rapamycin was even approved for use against a type of kidney cancer. Most importantly, in labs, it has demonstrated an ability to do something that no other drug has ever done before: extend the maximum lifespan of mammals.
- Rapamycin: How It Works — The reason rapamycin is used in so many areas is because it tends to slow down the process of cellular growth and division. In other words, it slows down the aging process. It acts directly on an important intracellular protein complex called mTOR. It is an mTOR inhibitor — it turns down mTOR temporarily. Why do we care about mTOR? Because this mechanism is one of the most important mediators of longevity at the cellular level. Additionally, rapamycin is highly “conserved,” meaning it has been passed on via natural selection to many different species, ranging from yeast to flies to worms and all the way up to humans.
- mTOR — mTOR is like the general contractor of a cell. It lies at the nexus of a long and complicated chain of upstream and downstream pathways that basically work together to regulate metabolism. It senses the presence of nutrients, especially certain amino acids, and it helps assemble proteins, the essential cellular building blocks. It basically has a finger in every major process in the cell.
- Quote (P. 77): “The job of mTOR is basically to balance an organism’s need to grow and reproduce against the availability of nutrients. When food is plentiful, mTOR is activated and the cell goes into growth mode, producing new proteins, and undergoing cell division. When nutrients are scarce, mTOR is suppressed and cells go into a kind of ‘recycling’ mode, breaking down cellular components and generally cleaning house. Cell division and growth slow down or stop, and reproduction is put on hold to allow the organism to conserve energy.”
- Rapamycin & Longevity — In 2009, a study came out and revealed that mice who were given rapamycin lived significantly longer on average than mice in the control group: 13% longer for females and 9% longer for males. It was a stunning result because no other drug had ever been shown to extend lifespan in a mammal. It was the equivalent of a pill that could make a 60-year-old woman live to the age of 95. The results were especially convincing because the experiment had been run by three different teams of researchers in three separate labs, using a total of 1,901 genetically diverse animals, and the results had been consistent across the board. Other labs also picked up these results and reproduced them in their own labs, which was a great sign for the validity of the study.
- Quote (P. 78): “The authors of the study, published in Nature, speculated that rapamycin might extend lifespan by postponing death from cancer, by retarding mechanisms of aging, or both. The real headline here, however, was that no other molecule had been shown to extend lifespan in a mammal. Ever.”
- Food Intake & Longevity — To scientists who study aging, the life-extending effect of rapamycin was really exciting, but it wasn’t a huge surprise. It appeared to confirm many centuries-worth of observations that linked how much we eat to how long we live. These observations go way back, but modern experiments have also proven, over and over, that reducing the food intake of lab animals could lengthen their lives.
- Quote (P. 82): “The real value of caloric restriction research lies in the insights it has contributed to our understanding of the aging process itself. Caloric restriction studies have helped to uncover critical cellular mechanisms related to nutrients and longevity. Reducing the amount of nutrients available to a cell seems to trigger a group of innate pathways that enhance the cell’s stress resistance and metabolic efficiency — all of them related, in some way, to mTOR.”
- Autophagy — Autophagy is a cellular recycling process that occurs when mTOR (and its cellular growth capabilities) is shut down, which happens when the body produces more of an enzyme called AMPK, which happens when you eat less or are exercising. When autophagy is at work, cells stop producing new proteins and instead break down old proteins and other cellular structures into their amino acid components, using the scavenged materials to build new ones. This is an important process for longevity.
- Quote (P. 83): “Autophagy is essential to life. If it shuts down completely, the organism dies… By cleansing ourselves of damaged proteins and other cellular junk, autophagy allows cells to run more cleanly and efficiently and helps make them more resistant to stress. But as we get older, autophagy declines… Thus, I find it fascinating that this very important cellular mechanism can be triggered by certain kinds of interventions, such as a temporary reduction in nutrients (as when we are exercising or fasting) — and the drug rapamycin.”
- Takeaway — Essentially, fasting and exercising reduce the amount of nutrients available in the body. When this happens, the enzyme AMPK shuts down mTOR, which in turn allows for autophagy to occur. Autophagy recycles waste in our cells and allows them to be more efficient. Although autophagy declines as we get older, it can be triggered by fasting and exercise. You can also take rapamycin to achieve autophagy because it also shuts down mTOR and its cellular growth capabilities.
- Quote (P. 83): “Autophagy is essential to life. If it shuts down completely, the organism dies… By cleansing ourselves of damaged proteins and other cellular junk, autophagy allows cells to run more cleanly and efficiently and helps make them more resistant to stress. But as we get older, autophagy declines… Thus, I find it fascinating that this very important cellular mechanism can be triggered by certain kinds of interventions, such as a temporary reduction in nutrients (as when we are exercising or fasting) — and the drug rapamycin.”
- Rapamycin: Where It Stands Today — Because one of rapamycin’s potential side effects is immune suppression, it hasn’t been tested on humans, despite being a promising longevity drug for all of the reasons discussed in this chapter. Currently, transplant patients and a small but growing group of others around the world take it. There is a clinical study going on right now that is testing rapamycin on companion dogs, with results expected in 2026. Attia has been taking rapamycin for three years.
- Chapter Takeaway — Rapamycin is a drug that has shown extreme promise when it comes to longevity, but it is still a bit of a mystery because it hasn’t been tested on humans. The drug is an mTOR inhibitor, meaning it helps promote autophagy and slows down the cellular growth process in your body. Autophagy can also be sparked through nutrient deficiency, which can be accomplished by fasting and exercising.
Ch. 6: The Crisis of Abundance
- NASH & NAFLD — These are metabolic diseases of the liver that often fly under the radar of patients and doctors because they show no symptoms. They are basically two stages of the same disease. NAFLD is the first stage, caused by more fat entering the liver or being produced than exiting it. NASH is NAFLD plus inflammation. The inflammation causes scarring in the liver. Weight loss usually allows you to stop NASH from getting serious. But if NASH isn’t stopped and the scarring continues without intervention, it can lead to cirrhosis, which is far more serious and can cause you to have liver failure. You would need a liver transplant.
- ALT — Rising ALT in a blood test is often the first clue that something is wrong with your liver. The “acceptable” range for ALT is below 45 IU/L for men. But that’s not good enough. You should shoot for under 33 or 30 ALT in your blood test.
- Quote (P. 93): “I care about NAFLD and NASH — and you should too — because they represent the tip of the iceberg of a global epidemic of metabolic disorders, ranging from insulin resistance to Type 2 diabetes. Type 2 diabetes is technically a distinct disease, defined very clearly by glucose metrics, but I view it as simply the last stop on a railway line passing through several other stations, including hyperinsulinemia, prediabetes, and NAFLD/NASH. If you find yourself anywhere on this train line, even in the early stages of NAFLD, you are likely also en route to one or more of the other three Horsemen diseases (cardiovascular disease, cancer, and Alzheimer’s disease). As we will see in the next few chapters, metabolic dysfunction (see the metabolic syndrome notes below) vastly increases your risk for all of these. So you can’t fight the Horsemen without taking on metabolic dysfunction first.”
- Average Isn’t Optimal — As the general population has become heavier and more unhealthy over the years and decades, “average” tests or readings shouldn’t be viewed as satisfactory. Average isn’t optimal anymore. Many patients and doctors don’t pay attention to their readings when they fall in the “average” category. I’m reality, you should strive for better than average readings. The ALT note above is a good example.
- Metabolic Syndrome (MetSyn) — It doesn’t matter if you are thick or thin, the criteria of metabolic syndrome applies to everyone. Whether you are obese or not doesn’t matter; studies have shown that one-third of obese people are metabolically healthy. It is critical to have a healthy metabolic system. The following five criteria make up metabolic syndrome. If you meet three or more of these criteria, then you have metabolic syndrome. The more of these boxes you check, the more at risk you are for cardiovascular events like heart attack.
- 1 — High blood pressure (>130/85)
- 2 — High triglycerides / Fat cells (>150 mg/dL)
- 3 — Low HDL cholesterol (<40 mg/dL in men)
- 4 — Central adiposity / abdominal fat (waist circumference > 40 inches in men)
- 5 — Elevated fasting glucose (>110 mg/dL)
- Quote (P. 95): “Out of a conservatively estimated 100 million Americans who meet the criteria for the metabolic syndrome (i.e., metabolically un-healthy), almost exactly one-third are not obese. Many of these folks are overweight by BMI (25-29.9), but nearly 10 million Americans are normal weight (BMI 19-24.9) but metabolically unhealthy. Some research suggests that these people might be in the most serious danger. A large meta-analysis of studies with a mean follow-up time of 11.5 years showed that people in this category have more than triple the risk of all-cause mortality and/or cardiovascular events than metabolically healthy normal-weight individuals. Meanwhile, the metabolically healthy but obese subjects in these studies were not at significantly increased risk. The takeaway is that it’s not only obesity that drives bad health outcomes: its metabolic dysfunction. That’s what we’re concerned with here.”
- Metabolism — Metabolism is the process by which we take in nutrients and break them down for use in the body. In someone who is metabolically healthy, those nutrients are processed and sent to their proper destinations. But when someone is metabolically unhealthy, many of the calories they consume end up where they are not needed (at best) or outright harmful (at worst). If you eat a doughnut, for example, there are two ways those calories can be processed depending on how healthy your metabolic system is:
- Converted to Glycogen — The calories can be converted to glycogen, the storage form of glucose, and used for activity in the near term. An adult male can store enough glycogen for about two hours worth of vigorous exercise before more is needed. The calories are basically used as fuel. The way this works is the liver converts the glycogen to glucose and then releases it in the body as needed to maintain blood glucose levels at a steady rate. This is an incredibly delicate task: an average adult male will have about 5 grams of glucose circulating in his bloodstream at any given time. That five grams won’t last more than a few minutes, as glucose is used up by the muscles and especially the brain, so the liver has to continually feed in more, distributing it precisely to maintain a more or less constant level. Consider that five grams of glucose, spread out across one’s entire circulatory system is normal, while seven grams means you have diabetes. The liver is an amazing organ!
- Stored as Fat — The other destination for the doughnut’s calories is stored fat. The decision of where to put the energy from the doughnut is made via hormones, especially insulin, which is secreted by the pancreas, when the body senses the presence of glucose, which is the final product of most carbohydrates (such as those in a doughnut). Insulin shuttles the glucose to where it’s needed while not screwing up the glucose balance in the body that the liver is orchestrating. Unless you are exercising hard, the excess energy from the doughnut will go to fat cells (triglycerides). If you are exercising hard, the energy will be consumed immediately by your muscles.
- Fat & Subcutaneous Fat — Subcutaneous fat — the layer of fat just below our skin —isn’t bad. It’s one of the safest places to store excess energy. Fat acts like a metabolic buffer zone, absorbing excess energy and storing it safely until it is needed. If we eat extra doughnuts, those calories are stored in our subcutaneous fat; when we go on a long hike or swim, some of that fat is then released for use by the muscles. This fat dynamic goes on continuously. As long as you haven’t exceeded your own fat storage capacity, things are pretty much fine.
- Excess Fat & The Bathtub— If you consume energy in excess of your needs, your subcutaneous fat cells will slowly fill up, particularly if little of that stored energy is being utilized. When someone reaches the limit of their capacity to store energy in their subcutaneous fat, yet they continue to take on excess calories, all that energy still has to go somewhere. It’s almost as if you have a bathtub, and you’re filling it up from the faucet. If you keep the faucet running even after the tub is full and the drain is closed, water begins spilling over the rim of the tub, flowing into places where it’s not wanted or needed, like onto the bathroom floor, into the heating vents or down the stairs. It’s the same with excess fat. As more calories flood into your subcutaneous fat tissue, it eventually reaches capacity and the surplus begins spilling over into other areas of your body: into your blood, as excess triglycerides; into your liver, contributing to NAFLD; into your muscle tissue, contributing directly to insulin resistance in the muscle; and even around your heart and your pancreas. None of these, obviously, are ideal places for fat to collect; NAFLD is just one of many undesirable consequences of this fat spillover.
- Genetics — Based on genetics, some people have higher and lower fat-storage capacity. Going back to the tub analogy, some people have fat-storage capacity equivalent to a regular bathtub, while others may be closer to a full-sized jacuzzi or hot tub. Others might only have the equivalent of a five-gallon bucket. It also obviously matters how much water is flowing into the tub via the faucet (as calories from food) and how much is flowing out via the drain (exercise). This explains in part why some people can be obese but metabolically healthy, while others can appear skinny while still walking around with three or more markers of metabolic syndrome.
- Abdominal Fat & The DEXA Scan — Abdominal fat, or visceral fat, is some of the worst fat you can have because it is fat that is accumulating between your organs. You can’t necessarily see or feel it — it’s wrapped around your inner organs deep in the abdominal section of your body. This fat is linked to increased risk of both cancer and cardiovascular disease. This type of fat should be monitored closely via an annual DEXA scan. This is one of the “bad” places excess calories/fat can go.
- Quote (P. 100): “It doesn’t take much visceral fat to cause problems. Let’s say you are a 40-year-old man who weighs 200 pounds. If you have 20% body fat, making you more or less average (50th percentile) for your age and sex, that means you are carrying 40 pounds of fat throughout your body. Even if just 4.5 pounds of that is visceral fat, you would be considered at exceptionally high risk for cardiovascular disease and Type 2 diabetes, in the top-5 percent of risk for your age and sex. This is why I insist my patients undergo a DEXA scan annually — and I am far more interested in their visceral fat than their total body fat.”
- Insulin — Insulin is a naturally occurring hormone made by your pancreas that helps your body use sugar for energy. It shuttles glucose to where it needs to be and helps bring down glucose levels to where they need to be. If your pancreas doesn’t work as it should, it may not make or release the insulin you need to control your blood sugars/glucose in your body, resulting in diabetes. Put simply, when glucose is up in the body, insulin is released to bring it down. The higher your blood glucose (via a bad diet consisting of sugar and simple carbs), the more insulin is being created and released by the pancreas. There comes a point (if blood glucose is constantly too high) where the pancreas gets tired and can’t produce enough insulin to maintain blood glucose balance. This is when diabetes occurs and you need to take insulin.
- Insulin Resistance — One of the first places excess energy/fat will cause problems is in your muscles by causing insulin resistance. Microscopic fat droplets wiggle in between you muscle fibers and even inside your muscles. This is where insulin resistance begins. Insulin resistance is when cells in your muscles, fat, and liver don’t respond well to insulin and can’t easily take up glucose from your blood. As a result, your pancreas makes more insulin to help glucose enter your cells. It’s one of the big contributors to diabetes. It’s worth noting that one key ingredient in this process seems to be inactivity. If a person is not physically active, and they are not consuming energy via their muscles, then this fat-spillover-driven insulin resistance develops much more quickly.
- Insulin Resistance: A Visual — Insulin resistance occurs when cells, initially muscle cells, have stopped listening to insulin’s signals, but another way to visualize it is to imagine the cell as a balloon being blown up with air. Eventually, the balloon expands to the point where it gets more difficult to force more air inside. You have to blow harder and harder. This is where insulin comes in, to help facilitate the process of blowing air into the balloon. The pancreas begins to secrete even more insulin, to try to remove excess glucose from the bloodstream and cram it into cells. For the time being it works, and blood glucose levels remain normal, but eventually you reach a limit where the “balloon” (cells) cannot accept any more “air” (glucose). This is when the trouble shows up on a standard blood test, as fasting blood glucose begins to rise. This means you have high insulin levels and high blood glucose, and your cells are shutting the gates to glucose entry. If things continue in this way, then the pancreas becomes fatigued and less able to mount an insulin response. This is made worse by the fat now residing in the pancreas itself. You can see the vicious spiral forming here: fat spillover helps initiate insulin resistance, which results in the accumulation of still more fat, eventually impairing our ability to store calories as anything other than fat.
- Rise of Diabetes — Diabetes is diagnosed when your blood glucose levels are too high, and didn’t used to be a problem for people in ancient times. Our modern diet, in particular consuming more fructose, has contributed to the disease’s rise. It is technically the 7th or 8th leading cause of death, but it’s far more serious than that because it has features, like insulin resistance, that lead to cancer, heart disease, and more.
- Quote (P. 103): “Patients with diabetes have a much greater risk of cardiovascular disease, as well as cancer and Alzheimer’s disease and other dementias; one could argue that diabetes with related metabolic dysfunction is one thing that all these conditions have in common. This is why I place such emphasis on metabolic health, and why I have long been concerned about the epidemic of metabolic disease not only in the United States but around the world.”
- Fructose & Human Metabolism — Fructose is a very powerful driver of metabolic dysfunction if consumed to excess. It is a form of sugar that is found in nearly all fruits, but humans have a unique ability to easily turn calories from fructose into fat. Avoid high fructose corn syrup and other unnatural sources at all costs! Fruits are OK because the fructose from those are also joined by water and fiber.
- Fructose & Uric Acid — In humans, fructose is metabolized differently than other sugars. When we metabolize fructose, along with certain other types of foods, it produces large amounts of uric acid, which is best known as a cause of gout, but which has also been associated with elevated blood pressure. Uric acid is why fructose is so bad for us. Other mammals possess an enzyme called uricase, which helps them clear uric acid. But humans lack this enzyme, so uric acid builds up in the body, with all of its negative consequences. Uric acid is so bad because it promotes fat storage (it evolved in us to help us put on fat to survive the winter, and we lack the enzyme uricase) and it elevates blood pressure.
- Quote (P. 106): “I test my patients’ levels of uric acid, not only because high levels may promote fat storage but also because it is linked to high blood pressure. High uric acid is an early warning sign that we need to address a patient’s metabolic health, their diet, or both.”
- Quote (P. 106): “The mechanisms are a bit complicated, but the bottom line is that even though it is rich in energy, fructose basically tricks our metabolism into thinking that we are depleting energy — and need to take in more food and store more energy as fat.”
- Biomarkers to Watch — Attia has several “biomarkers” or signs that he looks for in his patients. If any of these are off, it’s a sign to him that metabolic syndrome is occurring. Because the other three Horsemen (heart disease, cancer, and Alzheimer’s) also have poor metabolic health in common, the metabolism is one of the most important things to watch. Insulin level is the No. 1 thing Attia looks for and monitors in patients.
- Quote (P. 108): “In my patients, I monitor several biomarkers related to metabolism, keeping a watchful eye for things like elevated uric acid, elevated homocysteine, chronic inflammation, and even mildly elevated ALT liver enzymes. Lipoproteins, which we will discuss in detail in the next chapter, are also important, especially tri-glycerides; I watch the ratio of triglycerides to HDL cholesterol (it should be less than 2:1 or better yet, less than 1:1), as well as levels of VLDL, a lipoprotein that carries triglycerides all of which may show up many years before a patient would meet the textbook definition of metabolic syndrome.”
- Quote (P. 109): “One test that I like to give patients is the oral glucose tolerance test, or OGTT, where the patient swallows ten ounces of a sickly-sweet, almost un-drinkable beverage called Glucola that contains seventy-five grams of pure glucose, or about twice as much sugar as in a regular Coca-Cola. We then measure the patient’s glucose and their insulin, every 30 minutes over the next two hours. Typically, their blood glucose levels will rise, followed by a peak in insulin, but then the glucose will steadily decrease as insulin does its job and removes it from circulation. On the surface, this is fine: insulin has done its job and brought glucose under control. But the insulin in someone at the early stages of insulin resistance will rise very dramatically in the first 30 minutes and then remain elevated, or even rise further, over the next hour. This postprandial insulin spike is one of the biggest early warning signs that all is not well.”
- Metabolic Health Is Crucial — In many ways, good health and longevity starts with your metabolic health. You have to take this part of your health seriously. In addition to Type 2 diabetes, heart disease, cancer, and Alzheimer’s disease all generally have poor metabolic health in common. Monitor this area of your health carefully.
- Quote (P. 109): “Studies have found that insulin resistance itself is associated with huge increases in one’s risk of cancer (up to twelvefold), Alzheimer’s disease (fivefold), and death from cardiovascular disease (almost sixfold) — all of which underscores why addressing, and ideally preventing, metabolic dysfunction is a cornerstone of my approach to longevity.”
- Quote (P. 110): “In the next three chapters, we will explore the three other major diseases of aging-cardiovascular disease, cancer, and neurodegenerative diseases — all of which are fueled in some way by metabolic dysfunction. It will hopefully become clear to you, as it is to me, that the logical first step in our quest to delay death is to get our metabolic house in order. The good news is that we have tremendous agency over this. Changing how we exercise, what we eat, and how we sleep can completely turn the tables in our favor.”
- Chapter Takeaway — Living a longer, higher-quality life starts with taking care of your metabolic health. Although you don’t technically have metabolic syndrome if you don’t check three of its five criteria, you should strive to avoid any of the criteria. The reason metabolic health is so important is that it is one of the common denominators between Type 2 diabetes, heart disease, cancer, and Alzheimer’s disease. Extra visceral (abdominal fat) and insulin resistance are very bad.
Ch. 7: The Ticker
- No. 1 Killer — Heart disease and stroke, which lumped together are referred to as atherosclerotic cardiovascular disease, is the leading cause of death globally. It kills about 2,300 people in the U.S. every day, according to the CDC. Although heart disease is the No. 1 killer globally, it is also more easily prevented than cancer and Alzheimer’s disease. We know a lot about this disease, including how it develops and ways to prevent or delay it.
- Quote (P. 115): “Put bluntly, this should be the tenth leading cause of death, not the first.”
- Surprising CT Scan — In his mid-30s, Attia had a CT scan of his heart that revealed a calcium score of 6. For someone his age, the number should have been 0. In people with severe heart disease, the number would be over 1,000. But a score of 6 meant he had more calcium in his arteries than 75-80% of people his age. This inspired him to learn more about heart disease and to take action against it.
- Heart & Vascular System — The heart is an amazing organ that pumps blood around the body every moment of our lives. When it stops, we stop. Our vascular system is also impressive — a web of veins, arteries, and capillaries that would stretch around the world twice if laid end to end. Each blood vessel allows vital substances to pass through its membranes and transports oxygen and nutrients to our tissues while carrying away waste. It also transports cholesterol molecules between cells.
- Cholesterol — Cholesterol is essential to life. It is required to produce some of the most important structures in the body, including cell membranes; hormones, such as testosterone, progesterone, estrogen, and cortisol; and bile acids, which are necessary for digesting food. All cells can make their own cholesterol, but 20% of our body’s large supply is found in the liver, which acts as a sort of cholesterol repository, shipping it out to cells that need it and receiving it back via the circulation. Overall blood cholesterol matters, but dietary cholesterol doesn’t matter.
- Quote (P. 116): “Well, some of it is — you know, the LDL or ‘bad’ cholesterol, which is inevitably counterpoised against the HDL, or ‘good’ cholesterol. I practically need to be restrained when I hear these terms (HDL and LDL cholesterol), because they’re so meaningless. And your ‘total cholesterol,’ the first number that people offer up when you’re talking about heart disease, is only slightly more relevant to your cardiovascular risk than the color of your eyes.”
- Cholesterol & Lipoproteins — Because cholesterol belongs to the lipid family (fats), it is not water soluble and thus cannot dissolve in our plasma like glucose or sodium and travel freely through our circulation. So it must be carted around in tiny particles called lipoproteins — the final ‘L’ in LDL and HDL — which act like little cargo submarines. These lipoproteins are part lipid and part protein; the protein is essentially the vessel that allows them to travel in our plasma while carrying their water insoluble cargo of lipids, including cholesterol, triglycerides, and phospholipids, plus vitamins and other proteins that need to be distributed to our tissues. There are two main kinds of lipoproteins:
- HDL — HDL lipoproteins carry more protein than fat. These are wrapped in a molecule called apolipoprotein A (apoA). This is often referred to as “good” cholesterol.
- LDL — LDL lipoproteins carry more fat than protein. These are wrapped in a molecule called apolipoprotein B (apoB). This is often referred to as “bad” cholesterol.
- Swapping Contents — HDL and LDL lipoproteins often “trade cargo.” This is why labeling HDL “good” cholesterol and LDL “bad” cholesterol doesn’t make sense. They interact and trade contents frequently. The cholesterol itself isn’t the problem; it’s the particles that transfer the cholesterol (the type of apolipoprotein) that are the issue.
- Cholesterol & Apolipoproteins — The bigger risk when it comes to heart disease has to do with the particle in which cholesterol is shuttled around in. HDL lipoproteins are wrapped in apoA, while LDL lipoproteins are wrapped in apoB. Every single lipoprotein that contributes to heart disease is wrapped in apoB. The most important thing to target when it comes to preventing heart disease is apoB; we have to get this as low as possible.
- Quote (P. 117): “This distinction may seem trivial, but it goes to the very root cause of atherosclerotic disease: every single lipoprotein that contributes to atherosclerosis — not only LDL but several others — carries this apoB protein signature.”
- Dietary Cholesterol Myth — The idea that dietary cholesterol is bad for you is a myth. In reality, most of the cholesterol in our circulation is produced by our own cells. There have been many research papers showing that dietary cholesterol may not have much to do with heart disease at all. Eating lots of saturated fat can increase levels of atherosclerosis — causing lipoproteins in blood, but most of the actual cholesterol we consume in our food ends up being pooped out. This misconception started because most of the major early research on cholesterol and heart disease had been conducted in rabbits, which have a unique ability to absorb cholesterol into their blood from food and form plaque. Humans do not have the same ability. In reality, your body makes cholesterol — when your dietary intake of cholesterol goes down, your body makes more. When you eat greater amounts of cholesterol, your body makes less. Because of this, foods high in dietary cholesterol have very little impact on overall blood cholesterol levels in most people. The real problem when it comes to LDL cholesterol and nutrition is saturated fat (e.g. beef, bacon, cheese, ham) and trans fat. These contribute to higher levels of LDL cholesterol in your blood, but dietary cholesterol isn’t a problem.
- Quote (P. 118): “The vast majority of the cholesterol in our circulation is actually produced by our own cells. Nevertheless, US dietary guidelines warned Americans away from consuming foods high in cholesterol for decades, and nutrition labels still inform American consumers about how much cholesterol is contained in each serving of packaged foods.”
- Quote (P. 118): “It took nearly two more decades before the advisory committee responsible for the US government dietary guidelines finally conceded (in 2015) that ‘cholesterol is not a nutrient of concern for overconsumption.’ Glad we settled that.”
- ‘Old Person’ Myth — The idea that heart disease only happens to old people is also a myth. Half of all cardiovascular events in men occur before the age of 65. Heart disease (atherosclerosis) is slow-moving and develops over time. The beginnings of it usually start early on in life and slowly build.
- Heart Disease Analogy: Breaking and Entering — The analogy of a “scene of a crime” shows how heart disease works. A blood vessel is the street. The arterial wall is represented by the houses that line each side of the street. The fence in front of the house is the endothelium, a delicate but critical layer of tissue that lines all of our arteries and veins. The endothelium is a barrier between the blood vessel (street) and the arterial wall (house) that controls the passage of materials and nutrients and white blood cells into and out of the bloodstream.
- Busy Street — The street is very busy, with a constant flow of blood cells and lipoproteins and plasma and everything else that our circulation carries, all brushing past the endothelium. Inevitably, some of these cholesterol-bearing lipoprotein particles will penetrate the barrier, into an area called the subendothelial space — or in our analogy, the front porch. Normally, this is fine, like guests stopping by for a visit. They enter, and then they leave. This is what HDL particles generally do: particles tagged with apoA (HDL) can cross the endothelial barrier easily in both directions, in and out. LDL particles and other particles with the apoB protein are far more prone to getting stuck inside. This is what actually makes HDL particles potentially “good” and LDL particles potentially “bad” — not the cholesterol inside, but the particles that carry it.
- LDL / apoB Trouble — The trouble starts when LDL particles stick in the arterial wall and subsequently become oxidized, meaning the cholesterol molecules they contain come into contact with a highly reactive molecule known as a reactive oxygen species, or ROS, the cause of oxidative stress. It’s the oxidation of the lipids on the LDL that kicks off the entire atherosclerotic cascade. Now that it is lodged in the subendothelial space and oxidized, rendering it somewhat toxic, the LDL/apoB particle stops behaving like a polite guest, refusing to leave — and inviting its friends, other LDLs, to join the party. Many of these also are retained and oxidized. The other big issue is the number of LDLs; more is bad.
- Quote (P. 121): “So to gauge the true extent of your risk, we have to know how many of these apo particles are circulating in your bloodstream. That number is much more relevant than the total quantity of cholesterol that these particles are carrying.”
- Endothelium Is Compromised — The endothelium being compromised by LDL/apoB is the reason heart disease occurs. When the endothelium is comprised, LDL/apoB lipoproteins are able to be oxidized and retained in the blood. They penetrate the arterial walls and more of their friends join them. They get “stuck” in there, which causes major problems. It is not an accident that the two biggest risk factors for heart disease, smoking and high blood pressure, cause damage to the endothelium.
- Endothelium Responds — When many LDL/apoB particles get stuck and oxidized inside the endothelium, they begin to clump together. In response, the endothelium “calls 911” and summons immune cells called monocytes to confront the intruders. These monocytes transform into a macrophage (often compared to a Pac-Man) and the macrophage eats the LDLs to remove them from the artery walls. But if the macrophage consumes too much cholesterol, it blows up into a foam cell. When these foam cells gather together, they form a “fatty streak” in the artery. These fatty streaks lead to plaque in the arteries. Autopsies of teenagers have shown these forms of plaque in their arteries, underscoring the point that heart disease starts very early.
- HDLs to the Rescue — HDLs also arrive on scene to help remove excess cholesterol from macrophages before they blow up. This is one of the reasons HDL cholesterol is considered “good cholesterol.” In the end, HDLs are not as well understood as LDLs. LDL-C (which is shown on your blood results) has been shown to have a strong link to cardiac events and are therefore more important to pay attention to.
- Foam Cells Ooze Together — As the foam cells begin to ooze together, they start to form plaque in our arteries. The artery wall tries to control the damage by putting a barrier around the plaque, which makes the situation worse.
- Plaque Grows — The plaque in your arteries begins to build and narrow the blood vessel, blocking the street and restricting blood flow through the vessel. If the plaque becomes unstable, eroding or even rupturing, you’ve really got problems. The damaged plaque may ultimately cause the formation of a clot, which can narrow and ultimately block the lumen of the blood vessel — or worse, break free and cause a heart attack or stroke. This is why we worry more about the noncalcified plaques than the calcified ones. Over time, the plaque builds and builds and builds until you have a complete blockage either from the plaque itself or a plaque-induced clot), often resulting in a heart attack or stroke.
- CT Angiogram — The events described in the “crime scene” above are fairly undetectable by a typical calcium scan. That’s why it’s good to get a CT angiogram, because it can help detect “soft” noncalcified plaque that is developing rather than only detecting “hard” calcified plaque that shows up on a calcium scan. The calcium scan can show you how much solid plaque has built up and calcified, but isn’t as good at showing the soft noncalcified plaque that is present in your body. The noncalcified plaque is ultimately more dangerous.
- Quote (P. 126): “And as my calcium score revealed, I already had a small, calcified plaque in the upper part of my left anterior descending (LAD) artery, one of the main arteries supplying my heart. There may have been other bad things happening there as well, but because I did not have a CT angiogram at this time, I had no sense of what kind of damage existed elsewhere in my coronary arteries. Anything shy of calcification is not identified by the calcium score.”
- Test apoB! — apoB, the particles that carry LDL cholesterol, are the enemy when it comes to heart disease. You have to get apoB levels down as much as possible. Your LDL-C readings can be fairly normal while your apoB numbers are sky high. The apoB test used to be rare 15 years ago. It is now more prevalent because the medical community is realizing the connection between apoB and heart disease. Get your aboB tested regularly! Attia has all of his patients tested for this regularly.
- Quote (P. 126): “Back then, nearly fifteen years ago, the apoB test (simply, measuring the concentration of apoB-tagged particles) was not commonly done. Since then, evidence has piled up pointing to apoB as far more predictive of cardiovascular disease than simply LDL-C, the standard ‘bad cholesterol’ measure.”
- Quote (P. 127): “According to an analysis published in JAMA Cardiology in 2021, each standard-deviation increase in apoB raises the risk of myocardial infarction by 38 percent in patients without a history of cardiac events or a diagnosis of cardiovascular disease (i.e. primary prevention). Thats a powerful correlation. Yet even now, the American Heart Association guidelines still favor LDL-C testing instead of apoB. I have all my patients tested for apoB regularly, and you should ask for the same test the next time you see your doctor.”
- Heart Disease Prerequisites — Heart disease usually develops when a person has (a) high apoB; (b) LDL oxidation (leading to plaques that a calcium scan picks up; and (c) inflammation. These are the three factors that, combined with something like high blood pressure, can lead to serious health issues.
- Quote (P. 127): “None of these is enough to guarantee that someone will develop heart disease, but all three are necessary to develop it. We are fortunate that many of these conditions can be modulated or nearly eliminated — including apoB, by the way — via lifestyle changes and medications. As we’ll discuss in the final section, I take a very hard line on lowering apoB, the particle that causes all this trouble. (In short: get it as low as possible, as early as possible).”
- Lp(a) & Bob Harper — You should get tested for Lp(a) at least once in awhile. It’s a deadly type of apoB particle that is fairly rare because it’s primarily hereditary. It busts through the endothelium and causes problems, usually in the form of a premature heart attack. Strangely, exercise doesn’t seem to help it, unlike LDL-C. Lp(a) is what caused Bob Harper’s — a famous personal trainer who is in great shape — heart attack in 2017 at the age of 52 (he survived!).
- Quote (P. 129): “When a patient comes to me and says their father or grandfather or aunt, or all three, died of ‘premature’ heart disease, elevated Lp(a) is the first thing I look for. It is the most prevalent hereditary risk factor for heart disease, and its danger is amplified by the fact that it is still largely flying under the radar of Medicine 2.0, although that is beginning to change. Most people have relatively small concentrations of this particle, but some individuals can have as much as one hundred times more than others. The variation is largely genetic, and an estimated 20 to 30 percent of the US population has levels high enough that they are at increased risk; also, people of African descent tend to have higher levels of Lp(a), on average, than Caucasians. This is why, if you have a history of premature heart attacks in your family, you should definitely ask for an Lp(a) test. We test every single patient for Lp(a) during their first blood draw. Because elevated Lp(a) is largely genetic, the test need only be done once (and cardiovascular disease guidelines are beginning to advise a once-a-lifetime test for it anyway).”
- apoB & Lp(a) — These are two of the most important readings to monitor throughout your life, especially apoB. Getting these two readings as low as possible is crucial to avoiding heart disease. ApoB particles are what break through the endothelium and create plaque along the artery walls. Lp(a) particles are part of the apoB family and are especially deadly, but they are primarily passed down from genetics.
- Quote (P. 130): “When I look at a patient’s blood panel for the first time, my eyes immediately dart to two numbers: apoB and Lp(a).”
- Quote (P. 131): “ApoB not only tells me the concentration of LDL particles (which, you’ll recall, is more predictive of disease than the concentration of cholesterol found within LDL particles, LDL-C), but it also captures the concentration of VLDL particles, which as members of the apoB family can also contribute to atherosclerosis (heart disease). Furthermore, even someone whose apoB is low can still have a dangerously elevated Lp(a).”
- Get apoB / LDL-C Down! — Again, you can’t get apoB (and its proxy LDL-C) down low enough. You want it as low as possible. Around a 100 mg/dL LDL-C reading is recommended, but you should shoot for somewhere in the 10-30 mg/dL range if possible. The reason you can strive to get apoB/LDL-C as low as possible is because the cholesterol contained in our lipoproteins (LDL & HDL) makes up just 15% of our body’s total pool of cholesterol. So low LDL-C readings are fine because there’s plenty of other cholesterol in the body to build structures, which is what cholesterol is supposed to do. Your HDL-C reading isn’t as important.
- Quote (P. 131): “Once you establish the central importance of apoB, the next question becomes, By how much does one need to lower it (or its proxy LDL-C) to achieve meaningful risk reduction? The various treatment guidelines specify target ranges for LDL-C, typically 100 mg/dL for patients at normal risk, or 70 mg/dL for high-risk individuals. In my view, this is still far too high. Simply put, I think you can’t lower apoB and LDL-C too much, provided there are no side effects from treatment. You want it as low as possible.”
- Quote (P. 133): “Lipoproteins aren’t the only significant risk factors for cardiovascular disease; as noted earlier, smoking and high blood pressure both damage the endothe-lum directly. Smoking cessation and blood pressure control are thus nonnegotiable first steps in reducing cardiovascular risk.”
- Getting apoB & LDL-C Down: Exercise, Nutrition, and Drugs — For most people, it takes a combination of exercise, nutrition, and drugs to get apoB/LDL-C down to where we want to see them (10-30 mg/dL). Diet and exercise aren’t enough by themselves. This is where statins and other lipid-lowering drugs come in. These are typically thought of as “cholesterol-lowering” medications, but they are better thought of in terms of increasing your body’s ability to clear apoB from blood circulation. That’s really our goal. Mostly this is done by amplifying the activity of LDL receptors (LDIR) in the liver, which absorb cholesterol from the bloodstream.
- Statins — These are designed to slow or inhibit cholesterol production and encourage the liver to increase the number of LDL receptors, which have the job of getting rid of LDLs in your blood. Attia recommends rosuvastatin (Crestor) along with a few other lipid-lowering drugs like ezetimibe (Zetia) and PCSK9 inhibitors. See below photos.
- Quote (P. 134): “I do think they (statins) are very helpful drugs for reducing apoB or LDL concentration in many patients… For those who can tolerate them (i.e. most people), I deploy them early and often.”
- Quote (P. 136): “For every seven people who are put on a statin at an early age, we could potentially save one life. The reason for this is simple math: risk is proportional to apoB exposure over time. The sooner we lower apoB exposure, thus lowering risk, the more the benefits compound over time and the greater our fundamental risk reduction.”
- Statins — These are designed to slow or inhibit cholesterol production and encourage the liver to increase the number of LDL receptors, which have the job of getting rid of LDLs in your blood. Attia recommends rosuvastatin (Crestor) along with a few other lipid-lowering drugs like ezetimibe (Zetia) and PCSK9 inhibitors. See below photos.
- Heart Disease & Time — Heart disease often develops in your body at a fairly young age and builds over time (often decades) until a major event occurs. Sometimes that’s when you’re 80, sometimes it’s when you’re 60. It could even happen at 30, 40, or 50. For these reasons, it is so important to start a prevention plan as early as possible. You have to work on lowering apoB / LPL-C readings as soon as possible. Get your blood pressure under control as well.
- Quote (P. 135): “Nearly all adults are coping with some degree of vascular damage, no matter how young and vital they may seem, or how pristine their arteries appear on scans. There is always damage, especially in regions of shear stress and elevated local blood pressure, such as curves and splits in the vasculature. Atherosclerosis is with us, in some form, throughout our life course.”
- Quote (P. 135): “Ten years is far too short a time horizon. If we want to reduce deaths from cardiovascular disease, we need to begin thinking about prevention in people in their forties and even thirties.”
- Quote (P. 136): “I no longer fear dying from cardiovascular disease the way I once did. My long, comprehensive program of prevention seems to have paid off. I feel a lot better now, at age fifty, than I did at age thirty-six, and my risk is a lot lower by any metric other than age. One major reason for this is that I started early, well before Medicine 2.0 would have suggested any intervention.”
- Quote (P. 136): “Sniderman and colleagues’ analysis found that looking at a thirty-year time frame rather than the standard ten years and taking aggressive precautionary measures early — like beginning statin treatment earlier in certain patients — could prevent hundreds of thousands more cardiac events, and by implication could save many lives.”
- Quote (P. 137): “Medicine 3.0 takes a much longer view — and more importantly seeks to identify and eliminate the primary causative agent in the disease process: apoB… Once you understand that apoB particles — LDL, VLDL, Lp(a) — are causally linked to ASCVD (heart disease), the game completely changes. The only way to stop the disease is to remove the cause (apoB), and the best time to do that is now.”
- Chapter Takeaway — Heart disease is the No. 1 killer in the world and it often develops very early in your life. Over time, as plaque builds up, it becomes deadly. The key to prevention is getting apoB and LDL-C readings down as much as possible, far lower than what is considered “normal.” ApoB lipoproteins carry LDL cholesterol and have the ability to break through your body’s endothelium, which is in charge of protecting the walls of your arteries. You have to get these readings down while also getting blood pressure under control. Blood pressure contributes to the mechanical breakdown of the endothelium. Exercise and good nutrition often aren’t enough — you should consider taking statins and other lipid-lowering drugs to get apoB/LDL-C readings down. Dietary cholesterol is perfectly fine because our bodies don’t absorb it very well, and we make much more cholesterol internally anyway.
Ch. 8: The Runaway Cell
- Cancer — Cancer is a genetic disease caused by an uncontrolled division of abnormal (cancer) cells in a part of the body. Cancer cells develop, divide rapidly, travel and spread to places in the body they shouldn’t be, and have an uncanny ability to avoid the detection of your immune system, which is responsible for detecting, targeting, and eliminating bad cells.
- Heart Disease vs. Cancer — Cancer is the second-leading cause of death in the U.S. behind heart disease. Together, these two conditions account for almost one in every two American deaths. The difference is that we understand the genesis and progression of heart disease fairly well, and we have some effective tools with which to prevent and treat it. As a result, mortality rates from heart disease have dropped by 2/3 since the middle of the 20th century. But cancer still kills Americans at almost exactly the same rate as it did 50 years ago. We just don’t understand cancer as well.
- Problems With Cancer — There are a few problems we face when it comes to treating and overcoming cancer. The fact that we don’t understand cancer as well as heart disease and some other conditions is part of what makes it so scary. We’ve made some strides since Richard Nixon declared the “War on Cancer” in 1971, but it’s been a tough battle to this point. Three of the biggest problems we face include:
- Limited Toolbox — Once cancer is established, we lack highly effective treatments for it. Our toolbox is limited. Surgery and radiation can be effective against local, solid-tumor cancers, but surgery isn’t really valuable when a cancer has metastasized (spread). Metastasized cancers can be slowed with chemo, but they often return and are more resistant than ever.
- Early Detection — Our ability to detect cancer at an early age remains very weak. Far too often, we discover tumors only when they cause other symptoms, by which point they are too locally advanced to be removed — or worse, the cancer has already spread to other parts of the body.
- Complexity — One of the biggest obstacles to a “cure” is the fact that cancer is not one single, simple, straightforward disease, but a condition with mind-boggling complexity. In the early 2000s, the National Cancer Institute attempted to sequence cancer tumor cells in hopes of finding the precise genetic changes that cause various kinds of cancers. They found that each tumor had more than 100 genetic changes driving each type of cancer, and those mutations were mostly completely random. Basically no two tumors are alike, which makes it very difficult to come up with treatment plans when somebody does have cancer.
- Addressing Cancer — Attia recommends a three-part strategy to dealing with cancer. The components of the plan, which will be discussed in this chapter, include:
- Prevention — Just like the other Four Horsemen, developing an aggressive prevention strategy is the best thing we can do to combat cancer.
- Treatments — We have to use newer and smarter treatments that target cancer’s weaknesses and exploit their vulnerability to new immune-based therapies. Immunotherapy has a lot of potential.
- Detection — We have to detect cancer as early as possible so our treatments can be used more effectively. The evidence is overwhelming that it’s much easier to deal with most cancers in their early stages. Things get difficult when the cancer spreads.
- Cancer Cells — Cancer cells are different than normal cells in two important ways. But beyond the two ways they differ from normal cells listed below, every variety of cancer is unique and different in its own way.
- Stop Growing! — Cancer cells don’t grow faster than normal cells — they just don’t stop growing when they are supposed to. They stop listening to the body’s signals that tell them to stop growing. In many people who have had cancer, their PTEN gene (which stops cells from growing and dividing) basically stops working. Cancer cells grow to the point of becoming a tumor.
- Metastasis — Cancer cells also differ from normal cells in that they have a weird ability to wander anywhere in the body. They travel to distant places in the body where they shouldn’t be, which causes problems. This is called metastasis, and it is what allows a cancerous cell in the breast to spread to the lung. This spreading is what turns many cancers from a manageable problem into a fatal disease.
- Spreading Cancer — Metastatic cancer is responsible for most cancer deaths. With a few exceptions, solid organ tumors typically kill you only when they spread to other organs. Breast cancer kills only when it becomes metastatic. Prostate cancer kills only when it becomes metastatic. You could live without either of those organs. So when someone dies from breast or prostate cancer, or even pancreatic or colon cancer, they died because the cancer spread to other, more critical organs such as the brain, the lungs, the liver, and bones. When cancer reaches those places, survival rates drop precipitously. What’s worse is that we don’t really know what causes cancer to spread.
- Chemotherapy — Chemotherapy is what we use to try to deal with cancer that has spread. Contrary to popular belief, it’s actually easy to kill cancer cells. The problem is being able to kill them while not harming normal cells. Traditional chemo borders on medicine and poison — the mustard gas used as a weapon during World War I was a direct precursor to some of the early chemo solutions, some of which are still in use. Unfortunately, chemo has a hard time keeping cancer down for good; when a patient enters remission, the cancer often comes back in some form.
- Chemotherapy & Side Effects — Chemo drugs are very harmful to cancer cells, which are rapidly dividing. They kill cancer cells pretty well. But other normal cells are also dividing rapidly, such as those lining the mouth, gut, hair follicles, and nails, which is why typical chemo causes side effects like hair loss and vomiting — the chemo is harming those cells as well. The problem is that chemo drugs aren’t able to target and kill only cancer cells. As a result, the drugs also kill many of the patient’s normal cells. This causes a ton of pain and discomfort. The other problem is that if a cancer cell manages to survive chemo, it mutates and becomes stronger.
- The Warburg Effect — The Warburg Effect is the observation that most cancer cells produce energy predominantly not through the ‘usual’ citric acid cycle and oxidative phosphorylation in the mitochondria as observed in normal cells, but through a less efficient process of ‘aerobic glycolysis’ consisting of a high level of glucose uptake and glycolysis followed by lactic acid fermentation taking place in the cytosol not the mitochondria. Cancer cells essentially eat way more glucose than a normal cell. This observation was first published by Otto Heinrich Warburg in the 1920s, and it gives insight into how cancer cells work and how they fuel their own rapid reproduction and growth. It also represents a kink in cancer’s armor.
- Obesity, Diabetes, and Cancer: A Link to Metabolic Health — The Warburg Effect and other factors are making it harder to ignore the link between cancer and metabolic dysfunction. As obesity and Type 2 diabetes have risen, they seem to be driving an increased risk for many types of cancers, including esophageal, liver, and pancreatic cancer. The American Cancer Society reports that excess weight is a leading factor for both cancer cases and deaths.
- Obesity — Globally, 12-13% of all cancer cases are attributed to obesity. Obesity itself is strongly associated with thirteen different types of cancers, including pancreatic, esophageal, renal, ovarian, and breast cancers, as well as multiple myeloma.
- Diabetes — Type 2 diabetes increases the risk of certain cancers, by as much as double in some cases (such as pancreatic and endometrial cancers).
- Quote (P. 152): “I suspect that the association between obesity, diabetes, and cancer is primarily driven by inflammation and growth factors such as insulin. Obesity, especially when accompanied by accumulation of visceral fat (and other fat outside of subcutaneous storage depots), helps promote inflammation, as dying fat cells secrete an array of inflammatory cytokines into the circulation. This chronic inflammation helps create an environment that could induce cells to become cancerous. It also contributes to the development of insulin resistance, causing insulin levels to creep upwards — and, as we’ll see shortly, insulin itself is a bad actor in cancer metabolism.”
- PI3K, Insulin, and the Warburg Effect — The P13K family of enzymes is why the Warburg Effect allows cancer cells to consume so much glucose. In effect, P13K opens the gate in a cell’s wall, allowing glucose to flood in and fuel its growth. Cancer cells in particular have an ability to turn up P13K activity while shutting down the cell’s PTEN, which is a tumor-surprising protein responsible for telling a cell to stop growing (discussed above). When P13K is activated by insulin, the cell is able to devour glucose at a great rate to fuel its growth. Thus, insulin acts as a kind of cancer enabler, accelerating growth. We need to monitor insulin and avoid insulin resistance at all costs.
- Quote (P. 153): “This (the relationship between PI3K and insulin) in turn suggests that metabolic therapies, including dietary manipulations that lower insulin levels, could potentially help slow the growth of some cancers and reduce cancer risk. There is already some evidence that tinkering with metabolism can affect cancer rates.”
- Takeaway — This observation, along with the fact that obesity has become linked with cancer, goes back to Attia’s point several times earlier in the book that metabolic health is crucial to the prevention of cancer, heart disease, and neurodegenerative conditions. Taking care of your metabolic health is where everything starts. Metabolic dysfunction appears to be factor in all of the Horsemen diseases.
- Quote (P. 154): “While it’s tricky to impossible to avoid or prevent the genetic mutations that help give rise to cancer, it is relatively easy to address the metabolic factors that feed it…What I am saying is that we don’t want to be anywhere on that spectrum of insulin resistance to type 2 diabetes, where our cancer risk is clearly elevated. To me, this is the low-hanging fruit of cancer prevention, right up there with quitting smoking. Getting our metabolic health in order is essential to our anticancer strategy.”
- Takeaway — Cancer is tough to stop with all of the genetic mutations of the cell that are in play, but we can at least take care of our metabolic health and therefore eliminate, or reduce, the metabolic factors that feed cancer cells and allow them to become even more powerful. We can do our part to take that the metabolic factors away from cancer cells.
- Quote (P. 153): “This (the relationship between PI3K and insulin) in turn suggests that metabolic therapies, including dietary manipulations that lower insulin levels, could potentially help slow the growth of some cancers and reduce cancer risk. There is already some evidence that tinkering with metabolism can affect cancer rates.”
- PI3K Inhibitors & Insulin — In order to prevent cancer cells from activating PI3K, therefore opening the cell gates and allowing glucose to flood in and help the cell grow, PI3K inhibitor drugs were produced. But they haven’t seemed to work well. The reason is that by turning down the insulin-related PI3K pathway, these drugs actually end up raising insulin and glucose levels in the body. Because glucose is blocked from entering the cell by the drug, more of it stays in the bloodstream. The body then thinks it needs to produce more insulin to get rid of all that glucose, possibly negating some of the effects of the drug.
- Lowering Insulin in Diet — In response, researchers began investigating whether PI3K inhibitor drugs paired with a diet that limited glucose (and therefore insulin) would help. A 2018 study found that it did. A diet that keeps glucose levels down and therefore limits insulin paired with PI3K inhibitor drugs has been shown to increase the effectiveness of the drugs on cancer cells. This finding is important because it shows that your metabolic state matters when it comes to cancer and cancer treatment.
- Cancer & Insulin Levels — The findings regarding PI3K inhibitors and diet, along with recent findings that fasting/caloric restriction programs help when fighting cancer prove that metabolic health matters and keeping insulin levels down is important. Again, metabolic health is really important for overall health and preventing the Horsemen diseases.
- The Immune System & Immunotherapies — Our immune system is programmed to distinguish “nonself” from “self” — that is, to recognize invading pathogens and foreign bodies among our own healthy native cells, and then to kill or neutralize the harmful agents. An immunotherapy is any therapy that tries to boost or harness the patient’s immune system to fight an infection or other condition (example: vaccines). The problem with trying to treat cancer this way is that while cancer cells are abnormal and dangerous, they are technically still our cells (“self”). They have cleverly evolved to hide from the immune system and specifically our T cells, the immune system’s assassins that would ordinarily kill foreign cells. Immunotherapies are still being harnessed and currently are only able to help a small number of patients, but there have been a few treatments that have shown some success. There is a lot of promise with immunotherapies.
- CAR-T — Interestingly, CAR-T treatment involves removing T cells (the immune system’s assassins) from a patient’s blood, loading them up with weapons to fight cancer cells by using genetic engineering to add antigen receptors specifically targeted to the patient’s tumors, and then infusing them back into the patient. The modified T cells then go in and wipe out the patient’s cancer. Unfortunately, this treatment has only been proven to be effective against B-cell lymphoma.
- Checkpoint Inhibitors — These drugs take the opposite approach by making cancer cells visible to the immune system. In other words, they “shine the light” on cancer cells, exposing them to normal T cells, which go in and kill the bad cancer cells. The drugs do this by blocking certain “checkpoints” that are in place to prevent T cells from going overboard and assassinating your normal cells. With these specific checkpoints blocked, cancer cells can’t hide under the radar; they get exposed and destroyed. One of the men who developed checkpoint inhibitors, James Allison, won a Nobel Prize for his work in 2018. These drugs also helped save the life of former President Jimmy Carter a few years ago.
- ACT — ACT is a class of immunotherapy whereby supplemental T cells are transferred into a patient, like adding reinforcements to an army, to bolster their ability to fight their own tumor. These T cells have been genetically programmed with antigens specifically targeted at the patient’s individual tumor type. It is similar to CAR-T cell therapy, but much broader in scope. As cancer grows, it quickly outruns the immune system’s ability to detect and kill it; there simply aren’t enough T cells to do the job. ACT attempts to overwhelm the cancer by sending in an army of targeted T cells.
- Cancer: An Internal War — When cancer cells are living and spreading inside you, it’s like a literal war is being waged in your body. The cancer cells are almost like spies — they do harm and they are largely undetected by your immune system and T cells. The cancer cells develop, multiply, and spread throughout the body, doing a ton of damage. Once the spreading has reached a certain point, they overwhelm your entire system to the point of death. At a certain point, there isn’t anything the body can do to combat all of the cancer cells. If a cancer isn’t detected fairly early, there’s not a lot that can be done. Immunotherapies have shown promise, but they are still a ways from being effective with a large number of patients.
- Early Detection — It is absolutely crucial to detect cancer in an early stage (Stage I) before it spreads. The fewer cancerous cells we have, the greater our likelihood of success. Outside of a few cancers that respond to immunotherapies, very few treatments can help an advanced form of metastatic cancer. Perhaps our best chance against cancer is a set of good prevention habits and early detection. When it comes to mindset around tests and scans for your health, keep in mind that it’s possible that not screening early and frequently is the most dangerous option.
- Quote (P. 166): “When cancers are detected early, in stage I, survival rates skyrocket. This is partly because of simple math: these earlier-stage cancers comprise fewer total cancerous cells, with fewer mutations, and thus are more vulnerable to treatment with the drugs that we do have, including some immunotherapies. I would go so far as to argue that early detection is our best hope for radically reducing cancer mortality.”
- Quote (P. 200): “Our primary tool for preventing cancer is to not smoke and to keep our metabolic health on track, but that’s a very broad-brush approach that only takes us so far. We still need to screen aggressively and hope we somehow manage to find any cancers that do develop before it’s too late.”
- Colon Cancer — Colon cancer is the No. 3 deadliest cancer behind lung (No. 1), breast/prostate (No. 2), and just ahead of pancreas (No. 4) and liver (No. 5) cancers. Of the five, colon cancer is the one we have the best shot at catching early because it grows in a relatively easy location to access and we can see it without any need for imaging techniques or surgical biopsy. Because it is so easily observed, we understand its progression from normal tissue to polyp to tumor.
- Colonoscopy — The purpose of the colonoscopy is to detect colon cancer by looking not only for full-fledged tumors, but also for polyps, which are growths that form in the lining of the colon. The recommended age to get a colonoscopy is age 45. We should be getting it by no later than age 40. And we should be doing follow-up colonoscopies every 2-3 years. Finding colon cancer early via a colonoscopy allows us to eliminate polyps or growths on the spot. It is one of the best tests you can possibly take in your cancer prevention toolkit.
- Quote (P. 169): “Not all polyps become cancer, but all colon cancers came from polyps. This is what makes a colonoscopy such a powerful tool. The endoscopist is able not only to spot potentially cancerous growths before they become dangerous but also to intervene on the spot, using instruments on the colonoscope to remove polyps for later examination. It combines screening and surgery into one procedure. It’s an amazing tool.”
- Quote (P. 170): “In my practice, we go further, typically encouraging average-risk individuals to get a colonoscopy by age forty — and even sooner if anything in their history suggests they may be at higher risk. We then repeat the procedure as often as every two to three years, depending on the findings from the previous colonoscopy.”
- External vs. Internal Cancers — It’s typically a lot easier to spot cancers that develop on the surface of the body than those that develop inside the body in our internal organs.
- External Cancers — Skin cancer and melanoma are examples of easily-detected cancers. Attia recommends an annual pap smear test to look for cervical cancer.
- Internal Cancers — Cancers that form inside the body are tough to identify at early stages. CT scans and MRIs typically only detect cancer once it’s already developed to a certain point. Ideally, we want to detect cancer even earlier than that.
- Lung Cancer — Lung cancer is the No. 1 killer among all cancers and can strike somebody that has never smoked before. About 15% of all lung cancer cases are in those who have never smoked. Attia recommends a low-dose CT scan to look for lung cancer.
- Early Detection Challenges — Testing and scanning for cancer isn’t the easiest thing. There are issues. For one, many of the scans available, like CT scans and MRIs, detect cancer only once it’s big enough to be seen. By that point, the odds might already be stacked against the patient. Second, many of the tests have been known to show false positives and false negatives. Before many tests are conducted, they have to be calibrated for sensitivity and specificity. When sensitivity is high, typically specificity is low. And vice versa. This is the yin-yang dynamic that can create false positives and false negatives. Emotional distress and the wrong course of treatment can occur when you get these misdiagnosis’. For these reasons, Attia typically doesn’t recommend a full-body MRI to look for cancer.
- Sensitivity — When the sensitivity of a certain test is high, it’s very good at finding cancer if cancer is there, hence very few false negatives.
- Specificity — When the specificity of a certain test is low, it’s not as good at telling you when you don’t have cancer, hence a lot of false positives.
- Quote (P. 173): “Historically, this has been done via imaging tests, such as CT scans, that enable us to ‘see’ a tumor. Radiation exposure notwithstanding, the main issue is that these tests don’t have very high resolution. It’s very difficult for these imaging technologies to discern a cancer smaller than about one centimeter in diameter. Even if you assume that this one-centimeter nodule is the only collection of cancer cells in the patient’s body (not a great assumption: the mouse in the trap is rarely the only one in the house), you’re still talking about more than a billion cancer cells by the time you reach the threshold of traditional detection. If we could catch these recurrent cancers sooner, we might have a better shot at keeping patients in remission.”
- Early Detection: A Combined Approach — Maybe the best approach to take given the challenges and tradeoffs that come with various cancer screenings and tests is a combined one. Pairing different diagnostic tests ranging from radiographic (e.g. MRI), direct visualization (e.g. colonoscopy), and biological/genetic (e.g. liquid biopsy) is likely the best way to correctly identify cancers at an early stage with the fewest false positives.
- Quote (P. 176): “Until we learn how to prevent or ‘cure’ cancer entirely, something I do not see happening in our lifetime, short of some miraculous breakthroughs, we need to focus far more energy on early detection of cancer, to enable better targeting of specific treatments at specific cancers while they are at their most vulnerable stages. This is why I’m such an advocate for early screening. It’s a simple truth that treating smaller tumors with fewer mutations is far easier than if we wait for the cancer to advance and potentially acquire mutations that help it evade our treatments. The only way to catch it early is with aggressive screening.”
- Chapter Takeaway — Cancer is really scary in part because we don’t know a lot about it and there aren’t too many really effective treatments available. When cancer strikes, a literal war has broken out in your body as cancer cells develop, multiply, spread, and attempt to overwhelm your entire system. They do all of this while being undetectable by your immune system and T cells. Immunotherapies have shown promise, but the best approach right now is a preventative one where you are taking care of your metabolic health and getting the appropriate tests/scans so you can detect any cancer you might have as early as possible before it spreads. Once it spreads, it’s tough.
Ch. 9: Chasing Memory
- Alzheimer’s Disease — In 1906, Dr. Alois Alzheimer, a psychiatrist who worked as a medical doctor at the state asylum in Frankfurt, Germany, performed an autopsy on a patient named Auguste Deter, a woman in her mid-50s, who had suffered from memory loss, hallucinations, aggression, and confusion in her final years. Alzheimer found that the neurons in her brain were tangled and spiderweb-like, coated with a strange white dental substance. A colleague later went on to call the condition “Alzheimer’s disease” after Alzheimer himself passed away in 1915. The disease typically develops slowly over decades and usually doesn’t become noticeable until at least age 65. For some reason, women tend to get Alzheimer’s far more than men.
- The Amyloid Hypothesis — In the 1980s, scientists determined that the strange “dental white substance” was a plaque called amyloid-beta. Since then, the assumption has been that the accumulation of amyloid-beta in the brain is what causes Alzheimer’s. The issue is that this hypothesis, and the drugs that have been developed to limit the accumulation of amyloid-beta in patients, haven’t yielded any meaningful results. In fact, more recent studies have found that the reverse can be true: some patients with all of the symptoms of Alzheimer’s disease have little to no amyloid in their brains. All of this has contributed to the confusion and lack of understanding with Alzheimer’s disease.
- Lack of Understanding — Alzheimer’s disease is maybe the most difficult to treat of the Four Horsemen because we have such a limited understanding of how any why it begins. We also don’t fully know how to prevent it, and we currently have no way to treat it once symptoms begin. It also doesn’t appear to be something that can be reversed once symptoms begin. These points all hold true for other neurodegenerative diseases like Lewy body dementia, ALS, Parkinson’s disease, and Huntington’s disease. Our best chance against these is to try to prevent them.
- APOE — As discussed in an earlier chapter, we do know that genetics play a big role in Alzheimer’s disease. APOE is a gene that has three variants: e2, e3, and e4. Having one or two copies of the e4 variant seems to significantly increase a person’s risk of developing Alzheimer’s disease and the other neurodegenerative diseases.
- Cognitive Reserve — Improving cognition by learning new things has been shown to help patients resist the symptoms of Alzheimer’s and the other neurodegenerative diseases. By doing this, you’re building “cognitive reserve,” which helps you develop your brain and memory. Learning difficult skills (e.g. learning a new language) and movements (e.g. learning to dance) is especially helpful because you’re forcing the brain to work and develop. In fact, exercise is the only intervention shown to delay the progression of Parkinson’s disease, which is primarily a movement-based disease.
- Blood Flow & Neurodegenerative Diseases — One theory that had roots in the 1920s but has gained steam over time is the idea that neurodegenerative diseases are caused by reduced blood flow to the brain. On autopsy, Alzheimer’s brains often display calcification of the blood vessels that feed the brain. The theory is that the blood vessels get tightened due to plaque buildup and result in less blood flow to the brain. Amyloid is then a result of that process and not the actual cause of Alzheimer’s. Studies that have shown strong links between Alzheimer’s disease and cardiovascular disease have helped build momentum for this theory.
- Glucose & Neurodegenerative Diseases — Yet another theory to counter the Amyloid Hypothesis holds that elevated blood glucose contributes to Alzheimer’s because it damages the blood vessels in the brain. This is exhibited in the fact that having Type 2 diabetes doubles or triples your risk of developing Alzheimer’s. In short, high blood glucose contributes to your risk of getting Alzheimer’s. On the other hand, insulin resistance is also a contributor because having it means your cells don’t accept glucose as they should and the reduced glucose metabolism that follows will then starve your brain neurons of the glucose they do need, which causes all kinds of problems for cognitive function.
- The Brain — The brain is a greedy organ. It makes up just 2 percent of our body weight, yet it accounts for about 20% of our total energy expenditure. Its eighty-six billion neurons each have between one thousand and ten thousand synapses connecting them to other neurons or target cells, creating our thoughts, our personalities, our memories, and the reasoning behind both our good and bad decision. The brain depends on a steady supply of glucose and oxygen. The brain is always the top priority for energy consumption and is the last organ to shut down — it first consumes glucose for fuel and then uses fat, muscle, other organs, and bone (in that order) if enough glucose isn’t available in the body.
- Prevention Is Key — Just like the other Horsemen, prevention is the key with neurodegenerative diseases. But in this case, prevention might be our only way of avoiding them. These diseases have a very long lifespan and develop over decades — dementia can progress unnoticed for years before symptoms occur. There are a battery of cognitive tests specialists can do to determine if a patient is on the early stages of a disease. A diagnosis is almost always observational, meaning there’s not really a scan that can spot something, with the exception of Alzheimer’s, which can be confirmed by testing for amyloid. A few strong preventative tactics include:
- Exercise — Exercise is, without a doubt, the No. 1 preventative tool against neurodegenerative diseases. The reason is that it targets two of the key causes of these diseases: exercise helps your vascular health (blood vessels) so you get good blood flow to the brain and it improves your metabolic health by helping us stay in glucose homeostasis (balanced glucose levels in the body) while avoiding insulin resistance. Endurance and strength training are important — one study conclusively found that people with stronger grip strength had a significantly reduced risk of developing dementia.
- Quote (P. 201): “I now tell patients that exercise is, full stop and hands down, the best tool we have in the neurodegeneration prevention tool kit.”
- Diet — Because metabolism plays such a big role in these diseases, a switch in diet could be useful. The brains of Alzheimer’s patients typically have a hard time using glucose for fuel. The brain’s ability to metabolize ketones and use them for fuel, however, does not decline. So it may make sense to diversify the brain’s fuel source from only glucose to glucose and ketones via ketogenic diet.
- Sleep — Sleep is a powerful tool against dementia and all of the Horsemen. When we’re asleep, our brain is healing itself and removing waste. We need to prioritize sleep.
- Flossing — There’s a surprising link between gum health and overall health, particularly heart health.
- Saunas — At least four sessions per week at 20 minutes per session at 179 degrees Fahrenheit seems to be the sweet spot to reduce the risk of Alzheimer’s by 65%. This type of sauna program also reduces heart disease risk by 50%.
- Exercise — Exercise is, without a doubt, the No. 1 preventative tool against neurodegenerative diseases. The reason is that it targets two of the key causes of these diseases: exercise helps your vascular health (blood vessels) so you get good blood flow to the brain and it improves your metabolic health by helping us stay in glucose homeostasis (balanced glucose levels in the body) while avoiding insulin resistance. Endurance and strength training are important — one study conclusively found that people with stronger grip strength had a significantly reduced risk of developing dementia.
- Chapter Takeaway — While neurodegenerative diseases typically don’t take hold until late in life, they tend to develop over time. Just like the other Four Horsemen, prevention is the key. Once symptoms begin to show, it’s hard to stop this one. Although we don’t fully understand how cognitive diseases work, there’s growing evidence that vascular and metabolic issues play a role in their development. By taking care of your heart health and metabolic health, you can reduce your risk of dementia and Alzheimer’s. Exercise is the No. 1 prevention tool here.
Ch. 10: Thinking Tactically
- Changing Environment — When it comes to health, the challenge we humans face in modern life is that our environment has changed dramatically over the last century or two — our food supply, eating habits, activity levels, and structure of our social networks — but our genes have barely changed at all. The notes from an earlier chapter about how fructose used to help us survive cold winters and now completely messes up our metabolic health because there’s so much of it in our food is a good example of this. Our genes no longer match our environment. That’s why we have to be smart about our health and our habits.
- Health Tactics — There are five core tactics we have to key in on to prevent the Four Horsemen and increase both our lifespan and healthspan. Optimizing and forming good habits in these five areas will significantly increase your chances of living a longer, healthier life.
- Exercise
- Nutritional Biochemistry
- Sleep
- Emotional Health
- Exogenous Molecules (Drugs)
- The Role of Data — As discussed in earlier chapters, data and tests play a crucial role in achieving good health. We have to be proactive about getting the right tests done and then we have to watch the numbers carefully. Data will give us good feedback and help inform our decisions about our health.
- Quote (P. 214): “We rely heavily on data in our decision-making and developing our tactics, including static biomarkers such as triglycerides and liver function tests, as well as dynamic biomarkers such as oral glucose tolerance tests, along with anthropometric measures such as data on body composition, visceral adipose tissue, bone density, and lean mass.”
- Takeaway — All of the tests mentioned above should be incorporated into your screening plan.
- Quote (P. 214): “We rely heavily on data in our decision-making and developing our tactics, including static biomarkers such as triglycerides and liver function tests, as well as dynamic biomarkers such as oral glucose tolerance tests, along with anthropometric measures such as data on body composition, visceral adipose tissue, bone density, and lean mass.”
- Chapter Takeaway — Now that we’ve read about all of the Four Horsemen, it’s time to take a look at the preventative tactics we can use to stay healthy. For the most part, all Four Horsemen are modern diseases that have popped up as our environment has changed over the past few centuries; our ancestors weren’t experiencing these problems.
Ch. 11: Exercise
- Exercise = Top Priority — More than any other tactic discussed in this book, exercise has the greatest impact on your overall physical, mental, and emotional health and longevity. Exercise delays the onset of chronic diseases across the board. There are scores of studies showing that exercise can lengthen your life by many years. There are so many benefits that come from exercise and weight training — it’s truly miraculous. You must prioritize exercise (cardio and lifting weights) in your life. No excuses. You have to find the time for this, no matter what is going on in your life. It’s an absolute must. You also have to find ways to maintain it for as long as possible as you age.
- Quote (P. 217): “More than any other tactical domain we discuss in this book, exercise has the greatest power to determine how you will live out the rest of your life.”
- Quote (P. 218): “So if you adopt only one new set of habits based on reading this book, it must be in the realm of exercise… Even a little bit of daily activity is much better than nothing. Going from zero weekly exercise to just 90 minutes per week can reduce your risk of dying from all causes by 14%. It’s very hard to find a drug that can do that.”
- Quote (P. 218): “Study after study has found that regular exercisers live as much as a decade longer than sedentary people. Not only do habitual runners and cyclists tend to live longer, but they stay in better health, with less morbidity from causes related to metabolic dysfunction.”
- Quote (P. 219): “The data on exercise tell us, with great clarity, that the more we do, the better off we will be.”
- Quote (P. 224): “The fitter you are, the lower your risk of death. Again, there is no other intervention, drug or otherwise, that can rival this magnitude of benefit. Exercise is so effective against diseases of aging — the Horsemen — that it has often been compared to medicine.”
- Cardiorespiratory (Aerobic) Fitness — The first component of exercise is aerobic fitness, which is how efficiently your body can deliver oxygen to your muscles and how efficiently your muscles can extract that oxygen, enabling you to run, walk, cycle, or swim long distances. It also comes into play in daily life in the form of physical stamina — the more aerobically fit you are, the more energy you will have for whatever you are doing.
- VO2 Max: A Measure of Aerobic Fitness — Many studies have shown that aerobic fitness, measured in terms of VO2 Max, is maybe the most powerful marker for longevity. VO2 Max is used to measure your aerobic fitness and represents the maximum rate at which a person can utilize oxygen to create ATP (the chemical “fuel” that powers our cells) to perform an action. The higher a person’s VO2 Max, the more oxygen they can consume to make ATP, and the faster they can ride or run. It’s measured while a person is exercising at their upper limit of effort. Most tests are conducted on a treadmill. The more oxygen your body is able to use, the higher your VO2 Max, which is shown as volume of oxygen a person can use, per kilogram of body weight, per minute. An average 45-year-old man will have a VO2 Max of 40 ml/kg/min, while an endurance athlete is around the high 60s. Tour de France riders are in the high 70s.
- Quote (P. 220): “Our human body has an amazing ability to respond to the demands placed on it. Let’s say I’m just sitting on the couch, watching a movie. At rest, someone my size might require about 300 ml of oxygen per minute in order to generate enough ATP, the chemical ‘fuel’ that powers our cells, to perform all the physiological functions necessary to stay alive and watch the movie. This is a pretty low level of energy demand, but if I go outside and jog around my neighborhood, the energy demands ramp up. My breathing quickens, and my heart rate accelerates to help me extract and utilize ever more oxygen from the air I breathe, in order to keep my muscles working. At this level of intensity, someone my size might require 2,500 to 3,000 ml of oxygen per minute, an eight-to-tenfold increase from when I was sitting on the couch. Now, if I start running up a hill as fast as I can, my body’s oxygen demand will increase from there: 4,000 ml, 4,500 ml, even 5,000 ml or more depending on the pace and my fitness level. The fitter I am, the more oxygen I can consume to make ATP, and the faster I can run up that hill. Eventually, I will reach the point at which I just can’t produce any more energy via oxygen-dependent pathways, and I’ll be forced to switch over lo less efficient, less sustainable ways of producing power, such as those used in sprinting. The amount of oxygen that I am using at this level of effort represents my VO2 Max.”
- VO2 Max & Longevity — Your VO2 Max is a number you should monitor closely and aim to improve over time. Several studies, including one by JAMA in 2018, have shown correlation between mortality and VO2 Max — someone with a below-average VO2 Max is at double the risk of all-cause mortality compared to someone in the top quartile. Someone at the very bottom VO2 Max quartile for their age group is four times likelier to die than someone in the top quartile, and five times more likely than someone in the elite quartile. Therefore, poor cardio fitness carries a greater relative risk to death than smoking. The more aerobically fit you are, the greater your chance for overall survival.
- Strength Training — The second component of exercise is strength training. Surprisingly, muscle is almost as powerfully correlated with longevity as aerobic fitness. A ten-year observational study of roughly 4,500 subjects ages 50 and older found that those with low muscle mass were at 40-50% greater risk of mortality than controls. The key is that muscle alone isn’t enough — the overall strength of those muscles matters. Your muscles have to be capable of generating force. Subjects with low muscle strength were at double the risk of death.
- Quote (P. 228): “This is why I place such an emphasis on weight training — and doing it now, no matter your age… Therefore, I will find a way to lift heavy weights in some way, shape, or form four times a week, no matter what else I am doing or where I might be traveling.”
- Falling — Muscle and strength support our bones and help us avoid awful falls at older ages. Falling is a surprisingly significant cause of death among older people. The CDC reports that 800,000 older people are hospitalized for falls every year. As you get old, remaining active, maintaining strength and muscle, and working on your balance can help you avoid falls, which are really bad because they cause immediate harm, and that harm then leads to inactivity and muscle loss.
- Exercise & Aging — One of the prime hallmarks of aging is that our physical capacity erodes. Our aerobic fitness declines for various reasons that begin with lower cardiac output, primarily due to reduced maximum heart rate. We lose strength and muscle mass with each passing decade, our bones grow fragile and our joints stiffen, and our balance falters, leading to falls that have awful near and long-term consequences.
- Maintain Activity & Muscle! — Activity levels and muscle mass remain relatively consistent as people age from their 20s and 30 into middle age, but both of these tend to decline steeply after age 65 and even more steeply after age 75. It’s like people fall off a cliff. By age 80, the average person will have lost 8 kilograms of muscle (18 lbs) from their body, compared to 4 kilograms (9 lbs) for people who remain active. The takeaway here is that continued muscle loss and inactivity literally puts our lives at risk. Just as with VO2 Max, you have to find ways to maintain muscle mass and strength at all costs.
- Centenarian Decathlon — Attia created this idea. The Centenarian Decathlon is about pinpointing a collection of 20-50 exercises and everyday tasks that you can do today and want to be able to do at age 80 or 90. Because our strength and aerobic fitness naturally decline over time, you have to be able to do these tasks at a much more strenuous level today in order to prepare yourself to be able to do them when you’re old. That’s the concept around this idea. Your goal is to train yourself to do the tasks at a high level today.
- Ex. Do five pull ups
- Ex. Walk with a 30-pound dumbbell in each hand for one minute
- Ex. Carry my own luggage
- Ex. Walk up a steep hill
- Chapter Takeaway — Exercise is the single most important tactic in your health arsenal. A dedicated exercise routine can significantly improve your healthspan and lifespan. You must prioritize exercise — both aerobic cardio work and weight training.
Ch. 12: Training 101
- Three Dimensions of Exercise — The three dimensions of exercise include (a) aerobic endurance, (b) strength, and (c) stability. All three of these are key to maintaining your health and strength as you age. It’s important to form a routine that incorporates all three of these elements.
- Aerobic Endurance — We’re referring to long, steady endurance work where we are training what physiologists call “Zone 2,” as well as maximum efforts where VO2 Max comes into play.
- Strength — Here we’re trying to build muscle and strength. These will help give us a good foundation as we get older.
- Stability & Balance — This one is often overlooked, but it is critical to long-term health. It’s important to train stability and balance so we can avoid injuries and falls as we get older.
- Mitochondria — Our mitochondria are the little “cellular engines” in our body that produce much of our energy. They are able to burn/use both glucose and fat to fuel our body and are important to our metabolic health. Healthy mitochondria are also important to maintaining the health of our brain and to controlling inflammation in our body. Our mitochondria can convert both glucose and fatty acids to energy — but while glucose can be metabolized in multiple different ways, fatty acids can be converted to energy only in the mitochondria. Typically, someone working at a lower relative intensity will be burning more fat, while at higher intensities they would rely more on glucose. Additionally, healthy mitochondria equals your body burns more fat than glucose. Unhealthy mitochondria equals your body burns more glucose than fat.
- Quote (P. 242): “It seems unjust, but the people who most need to burn their fat, the people with the most of it, are unable to unlock virtually any of that fat to use as energy, while the lean, well-trained professional athletes are able to do so easily because they possess greater metabolic flexibility (and healthier mitochondria).”
- Takeaway — People that are heavier tend to have worse mitochondrial health, meaning they burn glucose more than they burn fat. People who are health tend to have healthy mitochondrial health and therefore burn fat more than they burn glucose.
- Quote (P. 242): “It seems unjust, but the people who most need to burn their fat, the people with the most of it, are unable to unlock virtually any of that fat to use as energy, while the lean, well-trained professional athletes are able to do so easily because they possess greater metabolic flexibility (and healthier mitochondria).”
- Aerobic Efficiency: Zone 2 — Zone 2 is one of five levels of intensity used by endurance coaches and trainers, and is one of the two key areas of our aerobic fitness gameplan. It is long, steady endurance work done at somewhere between an easy to moderate pace. You can hold a conversation pretty comfortably in Zone 2 work. This form of exercise helps you safely dispose of excess glucose in the bloodstream and use fat as fuel.
- Zone 2 & Mitochondria — Zone 2 training significantly improves mitochondrial health, which in turn allows you to better utilize fat as fuel (as opposed to glucose) while you work. Having healthy mitochondria comes with a lot of benefits, which is part of the reason Zone 2 work is so important. In short, strong mitochondrial health allows you to better burn fat and use fat as fuel. When mitochondrial health is poor, you use glucose, rather than fat, as fuel. One recent study found that professional cyclists, who have outstanding mitochondrial health, use fat as fuel at a much higher rate than a nonactive person with poor mitochondrial health. The study found that the cyclists burned primarily fat while exercising, while the nonactive people were using primarily glucose.
- Quote (P. 237): “I am convinced that it is impossible to be healthy without also having healthy mitochondria, which is why I place a great deal of emphasis on long, steady endurance training in Zone 2.”
- Quote (P. 239): “As fundamental as Zone 2 training is for professional cyclists, however, San Villán believes that it’s even more important for nonathletes, for two reasons. First, it builds a base of endurance for anything else you do in life, whether that is riding your bike in a 100-mile century ride or playing with your kids or grandkids. The other reason is that he believes it plays a crucial role in preventing chronic disease by improving the health and efficiency of your mitochondria, which is why training aerobic endurance and efficiency (i.e. Zone 2 work) is the first element of my Centenarian Decathlon training program.”
- Zone 2 & Lactate — When we are working in Zone 2, we’re using Type 1 “slow twitch” muscle fibers. These feature a lot of mitochondria and are perfect for slow-paced endurance work. We can go for awhile. When we increase the pace, we begin to recruit Type 2 “fast twitch” muscle fibers, which generate more lactate in the process because of the way they create ATP. The problem is that lactate becomes lactic acid when paired with hydrogen ions, which is what causes the burn you feel. Therefore, Zone 2 work is the max level of effort we can maintain without accumulating lactate. We still produce it, but we’re able to match production of lactate with clearance of it. That allows us to go for awhile. Ideally, you want lactate levels to be constant and in the 1.7-2.0 millimoles range.
- Quote (P. 240): “I make a point of this (lactate and lactate ranges) because lactate is literally what defines Zone 2. It’s all about keeping lactate levels steady in this range, and the effort sustainable.”
- Other Benefits of Zone 2 Training & Mitochondrial Health — In addition to allowing your body to burn more fat than glucose, having good mitochondrial health is crucial to aging. As we get older, the amount and quality of our mitochondria decline. But when we do Zone 2 work, it stimulates the creation of new and more efficient mitochondria while eliminating dysfunctional ones. Yet another benefit of Zone 2 work is that, studies have shown, it allows your muscles to vacuum up glucose in your bloodstream. As outlined in previous chapters, chronic elevated glucose levels in your bloodstream lead to Type 2 diabetes, heart disease, and more. Zone 2 training initiates a sequence where your muscles are able to vacuum glucose out of your bloodstream, therefore avoiding this issue.
- Recommended Amount of Zone 2 Work — Most physiologists recommend a minimum of three hours of Zone 2 training per week to see meaningful benefits, which is about four 45-minute sessions. Although that’s a lot of time, Zone 2 work isn’t very strenuous and you can listen to educational podcasts to fill the time.
- Quote (P. 143): “I am so persuaded of the benefits of Zone 2 that it has become a cornerstone of my training plan. Four times a week, I will spend about an hour riding my stationary bike at my Zone 2 threshold.”
- Maximum Aerobic Output: VO2 Max — The second component of aerobic fitness is the VO2 Max. This is a much higher level of intensity — a hard, minutes-long effort. Oxygen consumption is the key to this — we want to get to our max rate of oxygen consumption. VO2 Max has been shown to be strongly correlated with longevity. Generally speaking, it tells you what you can and cannot do; the lower it goes, the less you can do. And VO2 Max tends to drop significantly as we get older, unless you train it and try to maintain it. Try to get your score tested annually and then try to improve it each year.
- Quote (P. 245): “The peak amount of oxygen you consume, typically close to the point at which you ‘fail,’ meaning the point where you just can’t keep going, yields your VO2 Max. We have all our patients do the test at least annually, and they almost all hate it. We then compare their results, normalized by weight, to the population of their age and sex.”
- VO2 Max: Push Yourself — Attia pushes his patients to train for as high a VO2 Max as possible. He tries to get them into the “elite” range (top 2%) for their age and sex, and then tries to get them to achieve the VO2 Max of someone two decades younger than them. The reason you want to train like this is because studies suggest that your VO2 Max will naturally decline by at least 10% per decade. When your VO2 Max drops, the number of things you can do drops. VO2 Max has also been shown to reduce your risk of all-death mortality significantly. By training your VO2 Max really hard now and by getting the number into a very elite category, you reduce your risk of dying, improve your aerobic fitness, enhance your overall health, and allow yourself to simply do more things as you get older. The goal here is to get your fitness to the level of someone decades younger than you.
- Quote (P. 247): “Once maximal oxygen consumption or VO2 Max drops below a certain level (typically about 18 mg/kg/min in men), it begins to threaten your ability to live on your own. Your engine is beginning to fail. This is why it’s so essential to train VO2 Max in addition to Zone 2.”
- Quote (P. 248): “The payoff is that increasing your VO2 Max makes you functionally younger. One study found that boosting elderly subjects’ VO2 Max by 6 ml/kg/min, or about 25%, was equivalent to subtracting 12 years from their age.”
- VO2 Max: How to Train It — The best way to train your VO2 Max is to supplement it with your Zone 2 work. You should try to do one VO2 Max session per week. A typical session involves going for four minutes at the maximum pace you can sustain for those four minutes. It’s not an all-out sprint, but it’s a very hard effort. Then ride or jog for four minutes easy to let your heart rate come down to under 100 bpm. Repeat this 4-6 times, then cool down. You can do this on a stationary bike, rower, or treadmill. Actually testing your VO2 Max requires going into a testing center — Attia recommends testing it once per year.
- Quote (P. 251): “You want to make sure that you get as close to fully recovered as possible before beginning the next set. If you fail to recover sufficiently between sets, you will not be able to reach your peak effort in the working sets and you’ll consequently miss the desired adaptation. Also, be sure to give yourself enough time to warm up and then cool down from this intense effort.”
- Aging & Type 2 Muscle Fibers — Sadly, our muscle mass begins to decline as early as our 30s. But we lose muscle strength about two or three times more quickly than we lose muscle mass. And we lose power (strength x speed) two to three times faster than we lose strength. This is because the biggest single change in the aging muscle is the atrophy of our fast twitch or Type 2 muscle fibers. Unless you train using heavy weights consistently, your Type 2 muscle fibers (and therefore your muscle, strength, and power) will wither away quickly as you age.
- Inactivity Is Dangerous — As you get older, inactivity becomes more and more costly. You will lose muscle and aerobic fitness very fast if you are inactive for even just 10 days. The rapid loss of muscle at older ages is called sarcopenia. And once you’ve lost muscle in old age, it’s next to impossible to get it back. You have to find ways to stay active and work on strength training as you get old.
- Bone Mineral Density (BMD) — Interestingly, bone density diminishes just as quickly as muscle mass as we age, peaking in our late 20s and slowly declining from there. Like muscle, we want to build this up as much as possible in our prime years, and then work hard to maintain it as we age. The reason? We want to avoid injury in our late years. We want sturdy bones. Attia recommends getting this tested every year.
- Quote (P. 254): “Another metric that we track closely in our patients is their bone density (technically, bone mineral density or BMD). We measure BMD in every patient, every year, looking at both of their hips and their lumbar spine using DEXA. This also measures body fat and lean mass, so it’s a useful tool across all of the body-composition domains that we care about.”
- Quote (P. 255): “The takeaway for readers here is that your BMD is important, demanding at least as much attention as muscle mass, so you should at least check your BMD every few years.”
- Strength Training: Building Armor — The purpose of strength training is protection in old age. We want to armor ourselves against injury and frailty by building our muscle, bone density, and strength now. Falls and injuries are a real risk as you get older — by building your muscle and strength now, you can protect yourself as you get older. We want to build now and have enough “reserves” for our later years. Building muscle and strength is almost impossible at older ages, so at that point it’s about maintaining what you already built in your younger years.
- Quote (P. 255): “Think of strength training as a form of retirement saving. Just as we want to retire with enough money saved up to sustain us for the rest of our lives, we want to reach older age with enough of a ‘reserve’ of muscle (and bone density) to protect us from injury and allow us to continue to pursue the activities that we enjoy. It is much better to save and invest and plan ahead, letting your wealth build gradually over decades, than to scramble to try to scrape together an individual retirement account in your late 50s and hope and pray that the stock market gods help you out. Like investing, strength training is also cumulative, its benefits compounding. The more of a reserve you build up, early on, the better off you will be in the long term.”
- Strength Training: ‘Carrying Stuff’ — Attia’s view on strength training is rooted in your ability to carry things. Improving your ability to carry and grip things will set you up nicely later in life by preventing injury and helping you execute day-to-day tasks when you’re older, whether that’s carrying objects, gripping rails, opening jars, lifting things over your head, or anything else. A few of the fundamentals of his strength training include:
- Grip Strength — Many studies suggest that grip strength, how hard you can squeeze something with one hand, predicts how long you will live. Low grip strength in your later years is not good. The farmer’s carry is a good way to train this. It involves walking around for a minute with dumbbells in your hands. Try to work up to holding half of your body weight in each hand (full body weight in total) for at least one minute. Hold the weight in each hand, arms at your sides, and walk. Keep your shoulder blades down and back. Another way to train grip strength is to hand from a pull-up bar for as long as possible. Men should try to hang for two minutes. This exercise shouldn’t be performed every day, just once in awhile.
- Eccentric Loading — Eccentric loading means loading the muscle as it is lengthening, such as when you lower a bicep curl. You want to focus on this down phase in all lifts. Try to go slow and really control the weight. Doing this, especially with leg exercises, helps us control our body when going down hills or stairs. This is important as we get older and falls become a real threat.
- Pulling Motions — Pulling motions, such as rows or pull-ups, help us develop grip strength and our ability to exert our will on the world. We need to be able to pull effectively as we get older; it’s an essential part of life.
- Hip-hinging Movements — Training your legs and butt via squats, deadlifts, step-ups helps you develop your lower body, which is your foundation. You need to have a strong base as you get older so you can get up from a sitting position, move around, and maintain your balance relatively easily.
- Rucking — Rucking is simply walking or hiking while carrying a weighted rucksack or backpack. It’s a staple of international military training, as soldiers must be able to carry weapons, food, and other supplies for long distances. Our ancestors used to engage in rucking every day out of pure necessity as they carried supplies and kills from camp-to-camp. We no longer need to do this in modern life. Attia engages in rucking for an hour 3-4 days per week. Shoot to carry a third of your body weight while walking/hiking around.
- Chapter Takeaway — Aerobic fitness, strength training, and stability work are the three key pillars of an effective exercise program. Working hard in all three of these areas now will come with big rewards down the line as you get older. Aerobically, you want to train both your Zone 2 fitness, as well as your VO2 Max. When it comes to strength, your mindset should be a focused on improving your ability to grip and carry things. Because your muscle, strength, and aerobic fitness decline naturally over time, it’s important to work hard on getting ahead now so you can maintain what you’ve built as you get old.
Ch. 13: The Gospel of Stability
- Stability Matters — Stability is the foundation of your health. It is about moving your body in a very efficient way that maximizes your energy forces and prevents injury. Being able to move your body correctly, with good posture and balance, is key as you get older. Good stability will help you avoid falls and other injuries.
- Quote (P. 265): “In my view, stability is essential to any kind of movement, particularly if our goal is to be able to keep doing that movement for years or decades. It is the foundation on which are twin pillars of cardiovascular fitness and strength must rest.”
- Quote (P. 267): “In sum, stability lets us create the most force in the safest manner possible, connecting our body’s different muscle groups with much less risk of injury to our joints, our soft tissue, and especially our vulnerable spine. The goal is to be strong, fluid, flexible, and agile as you move through your world.”
- Dynamic Neuromuscular Stabilization — The theory behind DNS is that the sequence of movements that young children undergo on their way to learning how to walk is not random or accidental, but part of a program of neuromuscular development that is essential to our ability to move correctly. The core belief behind DNS is that as we grow up and experience office/school life, we lose the natural, healthy, movement patterns that we developed as small children when we were learning how to move correctly. The point of DNS is to retrain our bodies, and our brains, in those patterns of perfect movement that we learned as little kids.
- Quote (P. 272): “Stability is an integral part of my training program. Twice a week, I spend an hour doing dedicated stability training, based on the principles of DNS, PRI, and other practices, with 10-15 minutes per day on the other days.”
- Breathing — Stability starts with the breath. Deep, steady breathing activates the calming parasympathetic nervous system, while rapid breathing triggers the opposite, the sympathetic nervous system, part of the fight-or-flight response. You want to breathe deep and through the nose. In DNS, they teach you to breathe while trying to feel like your entire abdominal area (not just the belly part) is expanding when you breathe. If you do this correctly, you will feel the entire circumference of your shorts expand evenly around your waist, even in the back, not just in the front.
- Quote (P. 276): “I practice this 360-degree abdominal breathing every day, not only in the gym but also while I am at my desk.”
- The Feet — Your feet are like the tires on a sports car; they are the most fundamental point of contact between our bodies and the world. They are the foundation for every move we make. They are also crucial to balance. DNS works on training the feet through “toe yoga” and a variety of other exercises.
- Chapter Takeaway — Stability, balance, and form in the gym and in everyday life are important and often overlooked. Your exercise routine should include some form of stability training. You want to build these up now so you can rely on them when you get older. Attia has many videos on how to perform certain movements here: https://peterattiamd.com/outlive/videos/
Ch. 14: Nutrition 3.0
- Lack of Understanding — Despite what some of the nutrition gurus on the internet and social media say, we still really don’t know how what we eat affects our health. There is no such thing as a “perfect diet.” The truth is, the best nutritional plan is the one that meets your needs. Paleo, low-carb, ketogenic, low-fat, vegan — none of those diets matter and none of them are correct. We all react to food molecules differently. It’s also important to understand that, although nutrition is vital, exercise is still king.
- Quote (P. 292): “Thanks to the poor quality of the science, we actually don’t know that much about how what we eat affects our health… It’s not about telling you what to eat; it’s about figuring out what works for your body and your goals — and, just as important, what you can stick to.”
- Quote (P. 295): “Nutritional interventions can be powerful tools with which to restore someone’s metabolic equilibrium and reduce risk of chronic disease. But can they extend and improve lifespan and healthspan, almost magically, the way exercise does? I’m no longer convinced that they can.”
- Quote (P. 318): “Some people will lose tremendous amounts of weight and improve their metabolic markers on a low-carbohydrate or ketogenic diet, while others will actually gain weight and see their lipid markers go haywire on the exact same diet. Conversely, some people might lose weight on a low-fat diet, while others will gain weight. I have seen this happen time and again in my own practice, where similar diets yield very different outcomes, depending on the individual.”
- Nutrition 3.0: Key Areas — In the end, nutrition is fairly simple: it’s about eating the right number of calories for your body, getting enough protein in your diet, obtaining the vitamins and minerals you need, and avoiding food diseases. In the end, we’re looking to address three areas:
- Calories — Are you undernourished or overnourished?
- Protein — Are you undermuscled or overmuscled?
- Metabolic Health — Are you metabolically healthy or not?
- Quote (P. 295): “The correlation between poor metabolic health and being overnourished and undermuscled is very high. Hence, for a majority of patients the goal is to reduce energy intake while adding lean mass. This means we need to find ways to get them to consume fewer calories while also increasing their protein intake, and to pair this with proper exercise. This is the most common problem we are trying to solve around nutrition.”
- Quote (P. 295): “Nutrition is relatively simple, actually. It boils down to a few basic rules: don’t eat too many calories, or too few; consume sufficient protein and essential fats; obtain the vitamins and minerals you need; and avoid pathogens like E. coli and toxins like mercury or lead. Beyond that, we know relatively little with complete certainty. Read that sentence again, please.”
- Problems with Nutrition Research — One of the big reasons we don’t know much about nutrition has to do with the research methods we use. We generally use two types of studies to study nutrition: epidemiology and clinical trials. These studies simply aren’t good enough to make conclusive arguments about food, which is so complex and is made up of thousands of chemical compounds in millions of combinations that interact with human physiology. In general, most studies about nutrition aren’t conclusive enough. What follows are a few problems with these studies.
- Too General — The problem with epidemiology studies is that they look at things with far too much of a general lens and they make too many assumptions. For example, one study seemed to show that people who drank Diet Coke were more at risk for issues like heart disease. The problem is that these types of studies fail to look at who would be drinking Diet Coke — people who tend to be overweight and are trying to limit their caloric and sugar intake. Because this group tends to be overweight, they are naturally at higher risk of disease in general. It doesn’t necessarily have anything to do with Diet Coke.
- Bad Raw Data — Data in epidemiology studies tend to be collected by having subjects fill out a form that asks them to list what they’ve eaten recently. It’s hard for anything to remember what they have eaten.
- Discipline — A big issue with clinical studies, which looks at Group X on a certain diet vs. Group Y on a different diet, is that you can’t trust that the subjects actually stuck to their prescribed diet throughout the process. If a person doesn’t follow the exact diet to a tee for the entire length of the study, it’s flawed. And there’s no way to guarantee subjects followed the diet, even if they said they did. Also, for these same discipline reasons, it’s hard to pull off a study that is long enough in duration to come up with conclusive findings.
- Individuality — At the end of the day, we are all different from a genetic standpoint. What affects one person won’t affect another. What works for one person’s diet, won’t work for another person with a different genetic makeup. Food is so complex, and its interaction with the human body and our individual genetic structure is hard to fully understand for every person. This makes nutritional studies hard to trust.
- Chapter Takeaway — Nutrition is fairly simple from an approach standpoint. It’s about getting the right amount of calories, getting enough protein, and obtaining the right amount of minerals and nutrients. Beyond that, we don’t know a whole lot about it because of how complex food and our individual genetic structures are. Epidemiology studies on nutrition are fairly useless, and clinical studies aren’t much better for a variety of reasons. All of this contributes to our lack of understanding when it comes to nutrition.
Ch. 15: Putting Nutritional Biochemistry into Action
- Standard American Diet (SAD) — The Standard American Diet includes way too many calories and grain-based products. This is part of the reason why we have an obesity issues in our country. The SAD diet disrupts the body’s metabolic equilibrium. It makes it very difficult for our body to control blood glucose levels (because the food we eat causes it to spike constantly), and it causes us to store fat when we should be utilizing it.
- Diets — When somebody goes on a diet, they are essentially trying to break away from SAD. No matter what diet somebody is on (e.g. Atkins, Paleo, Ketogenic, low-fat, etc.), they all are trying to get you to do one, or several, of three things, with eating fewer calories as the primary goal. The three strategies below are basically involved in every diet.
- Caloric Restriction (CR) — Eating less in total. Simply eating fewer calories than what your body requires. This is how you lose weight.
- Quote (P. 310): “From the standpoint of pure efficacy, CR is the winner, hands-down. This is how bodybuilders shed weight while holding on to muscle mass, and it also allows the most flexibility with food choices.”
- Dietary Restriction (DR) — Eating less of some particular element within the diet (e.g. meat, sugar, fats). Specifically targeting a certain element of the diet.
- Quote (P. 310): “It (DR) is conceptually simple: pick a type of food, and then don’t eat that food. It only works, obviously, if that food is both plentiful and significant enough that eliminating it will create a caloric deficit.”
- Time Restriction (TR) — Restricting eating to certain times, up to and including multi day fasting. This is basically what intermittent fasting is doing. This strategy is ultimately not great because it usually means you eat one or two times a day (or less), meaning you will not get enough protein to sustain your muscle mass. When this happens, you will lose muscle and might not even lose body fat — there’s a chance you’ll just alter your body composition for the worse (less muscle, same or more fat).
- Caloric Restriction (CR) — Eating less in total. Simply eating fewer calories than what your body requires. This is how you lose weight.
- Calories Matter — Calories, the amount of energy you take into your body, are probably the most important thing to watch when it comes to your nutrition. Many problems — metabolic dysfunction, heart disease, Alzheimer’s, cancer, and more — arise from eating more calories than your body needs. You put on weight and your fat stores build up. There are scores of research studies proving that people who count calories and limit them can and do lose weight. Calorie restriction has also been shown in several studies to increase lifespan, likely because you’re avoiding the Four Horsemen in the process of limiting caloric intake.
- Quote (P. 311): “I may be starting to sound like a broken record, but it should be obvious by now that many of the problems we want to address or avoid stem from consuming calories in excess of what we can use or safely store. If we take in more energy than we require, the surplus ends up in our adipose tissue, one way or another. If this imbalance continues, we exceed the capacity of our ‘safe’ subcutaneous fat tissue, and excess fat spills over into our liver, our viscera, and our muscles, as we discussed in chapter 6.”
- Quote (P. 311): “In prior chapters, we’ve seen how excess calories contribute to many chronic diseases, not only metabolic disorders but also heart disease, cancer, and Alzheimer’s disease.”
- Quality of Diet — Although you can lose weight eating whatever you want (e.g. junk food) as long as you aren’t eating more calories than your body requires, it’s best to eat a healthy diet with plenty of protein. You will feel better and perform better in every way.
- Quote (P. 312): “One slight advantage is that calorie counting is agnostic to food choices; you can eat whatever you want so long as you stay within your daily allowance… You can lose weight on a restricted-calorie diet consisting only of Snickers bars, but you will feel much better if you opt for steamed broccoli and chicken breasts instead.”
- Calories: The Monkey Studies — There were two 20+ year calorie-focused studies using monkeys as test subjects that have given us good insight on the value of not consuming too many calories and sticking to a high-quality diet. In both studies, there were a group of monkeys who were put on a caloric restriction diet, while the other group in both studies was allowed to eat anything they wanted. Together, the dueling monkey studies constitute one of the most rigorous experiments ever done about the complex relationship between nutrition and long-term health. The findings include:
- Metabolic Problems — Avoiding diabetes and related metabolic dysfunction, especially by eliminating or reducing junk food, is very important to longevity.
- Calories & Cancer — There appears to be a strong link between calories and cancer, the leading cause of death in the control monkeys (who were allowed to eat as much as they wanted) in both studies. The monkeys on a caloric deficit diet had a 50% lower incidence of cancer.
- Quality of Diet — The quality of the food you eat could be as important as the quantity. If you’re eating the SAD, then you should eat much less of it. The monkeys in one of the studies were eating far worse foods than the other study and died much sooner of diseases like diabetes, heart disease, and cancer than the monkeys with the quality diet.
- Dietary Restriction (DR) — Simply put, DR involves identifying one or two bogeymen in your nutritional world (e.g. carbs) and don’t eat it/them. By picking something that you eat a lot of currently, you increase your chances of reducing your overall caloric intake, which is ultimately the goal with DR — everything ultimately comes back to calories. It’s important to replace whatever you remove from your diet with something that doesn’t include even more calories, and it’s wise to not eliminate foods that are a high source of protein because protein is critical to muscle gain and retention. You also don’t want to use foods high in saturated fat as a replacement because those foods can send LDL-C and apoB readings up.
- Quote (P. 317): “We have too many choices, and too many delicious ways to take calories into our body. Hence the need for dietary restriction. We need to erect walls around what we can and cannot (or should not) eat.”
- Carbohydrates — One of the three core macronutrients alongside protein and fat, carbs are our primary energy source and are neither “good” nor “bad.” There are good complex carbs (e.g. fruit) and there are bad simple carbs (e.g. Twinkie). Think of carbs as glucose. The right amount of carbs (or glucose) will depend on the individual and depends largely on exercise. A pro athlete will be able to consume and burn many more carbs than the average person. Excessive carbohydrate intake can have spillover effects on apoB in the form of elevated triglycerides.
- Carbs & Glucose — In digestion, most carbohydrates are broken down to glucose, which is consumed by all cells to create energy in the form of ATP. Too much glucose, beyond what we need immediately, can be stored in the liver or muscles as glycogen for near-term use or tucked away as fat. This decision is made with the help of the hormone insulin, which is created by the pancreas and surges in response to the increase in blood glucose to try to get it down. As we learned earlier, the body tries to keep 5 grams of glucose in the bloodstream at all times. If the body can’t keep it lower than 7 grams consistently, you may have diabetes. You may also be on the path to the other Horsemen.
- Quote (P. 322): “We already know that it’s not good to consume excessive calories. In the form of carbohydrates, those extra calories can cause a multitude of problems, from NAFLD to insulin resistance to Type 2 diabetes, as we saw in chapter 6. We know that elevated blood glucose, over a long enough period of time, amplifies the risk of all the Horsemen. But there is also evidence suggesting that repeated blood glucose spikes, and the accompanying rise(s) in insulin, may have negative consequences in and of themselves.”
- Continuous Glucose Monitor (CGM) — This is a piece of technology that can help you monitor glucose levels in your bloodstream 24/7. You wear it on your arm and it sends real-time feedback on your glucose levels to your phone so you can figure out which foods elevate your glucose levels and which ones don’t. You can then better understand how to keep your glucose levels in a safe range, which will help you avoid all of the Horsemen. CGM is currently available only to diabetes patients, but is becoming more widely available. Eventually it will likely be available to everyone.
- Quote (P. 323): “CGM represents a huge improvement over the Medicine 2.0 standard of one fasting glucose test per year, which in my opinion tells you almost nothing of value.”
- CGM, Carbs, and Glucose — Ultimately it is crucial to keep glucose levels in a good range. Over time, high glucose levels contribute to the development of all of the Four Horsemen. Carbs increase glucose levels, which prompts the pancreas to release insulin into the bloodstream to bring it back down. The power of CGM is that it enables you to view your response to carbohydrate consumption in real time and make changes rapidly to flatten the curve and lower the average. Real-time blood glucose gives you a god look at likely insulin response, which we also want to minimize. CGM will help you understand which foods spike your glucose (and insulin) levels so you can avoid those foods on your diet.
- Quote (P. 324): “Typically, my healthy patients need to use CGM only for a month or two before they begin to understand what foods are spiking their glucose (and insulin) and how to adjust their eating pattern to obtain a more stable glucose curve. Once they have this knowledge, many of them no longer need CGM. It’s a worthwhile investment.”
- Quote (P. 325): “A 2011 study looking at 20,000 people, mostly without Type 2 diabetes, found that their risk of mortality increased monotonically with their average blood glucose levels. The higher their blood glucose, the greater their risk of death — even in the nondiabetic range of blood glucose. Another study in 2019 looked at the degree of variation in subjects’ blood glucose levels and found that the people in the highest quartile of glucose variability had a 2.67 times greater risk of mortality than those in the lowest (most stable) quartile. From these studies, it seems quite clear that we want to lower average blood glucose and reduce the amount of variability from day to day and hour to hour. CGM is a tool that can help us achieve that.”
- Takeaway — We want both lower average levels of glucose AND fewer big spikes in glucose levels. Both are important. Both can be better understood and addressed with CGM.
- Ideal Glucose Levels & Carb Timing — Not everyone needs to restrict carbohydrates; some people can handle more than others. Overall, Attia likes to keep average glucose at or below 100 mg/dL, with a standard deviation of less than 15 mg/dL. These are aggressive goals, but will help you avoid the Four Horsemen, each of which seem to feed off of elevated glucose in the bloodstream. In the end, we simply do not want high glucose and insulin levels. As for when to eat carbs, before workouts (because you then use them/burn them in your workout), after workouts, and in the morning are the best times. It’s best to try to minimize carb consumption at night.
- Quote (P. 327): “This doesn’t need to be an exercise in deprivation: one patient of mine gleefully confessed that his CGM, which he had only reluctantly agreed to wear, had given him a ‘superpower’ to cheat. By eating certain ‘forbidden’ types of carbohydrates only at certain times, either mixed with other foods or after exercising, he had figured out how he could hit his average glucose goals while still enjoying all the foods he loved. He was gaming his CGM, but he had also unwittingly discovered another rule of nutrition, which is that timing is important: If you scarf a large baked potato before working out, it will leave much less of a footprint on your daily glucose profile than if you eat it right before bedtime.”
- Glucose Levels & Sleep — Surprisingly, glucose levels spike with poor sleep. High stress (via your body’s cortisol release) also contributes to elevated glucose levels. Lack of sleep negatively affects your body’s ability to dispose of glucose the next day. If you are stressed out and not sleeping well, you really need to watch what you eat.
- Quote (P. 327): “Also, sleep disruption or reduction dramatically impairs glucose homeostasis over time. From years of experience with my own CGM and that of my patients, it still amazes me how much even one night of horrible sleep cripples our ability to dispose of glucose the next day.”
- Quote (P. 327): “Another surprising thing I’ve learned thanks to CGM is about what happens to a patient’s glucose levels during the night. If she goes to bed at, say, 80 mg/dL, but then her glucose ramps up to 110 for most of the night, that tells me that she is likely dealing with psychological stress. Stress prompts an elevation in cortisol, which in turn stimulates the liver to drip more glucose into circulation.”
- What Spikes Glucose Levels? — All carbs, but especially simple carbs that you find in highly processed food, are what send glucose levels up the most. Fructose (sugar) also spikes it. Foods high in protein and fat have almost no effect on glucose levels. Foods high in just protein (e.g. chicken) tend to elevate glucose levels very slightly. Protein shakes tend to come with a slight spike as well, especially if they have a lot of sugar.
- Quote (P. 328): “Not all carbs are created equal. The more refined the carb (think dinner roll, potato chips), the faster and higher the glucose spike. Less processed carbohydrates and those with more fiber, on the other hand, blunt the glucose impact. I try to eat more than 50 grams of fiber per day.”
- Protein — Protein, the second macronutrient, and amino acids are the building blocks of life. Without them, we can’t build or maintain the lean muscle mass we need. As we saw in a previous chapter, the older we get, the easier we lose muscle and the more difficult it is to rebuild it. That’s why protein is so important. Unlike carbs and fat, protein is not a primary source of energy — we don’t rely on it to make ATP (to fuel our cells) and we don’t store it like we store fat (in fat cells) and carbs/glucose (as glycogen). You don’t have to worry about eating too much protein — if you consume more protein than you can synthesize into lean mass, you will simply pee it out.
- Quote (P. 331): “Protein is all about structure. The 20 amino acids that make up proteins are the building blocks for our muscles, our enzymes, and many of the most important hormones in our body. They go into everything from growing and maintaining our hair, skin, and nails to helping form the antibodies in our immune system. On top of this, we must obtain nine of the twenty amino acids that we require from our diet, because we can’t synthesize them.”
- Quote (P. 347): “Protein is actually the most important macronutrient, the one macro that should not be compromised.”
- Daily Protein Target — The recommended amount of protein by the U.S. government is a joke. You need to shoot for at least one gram of protein per pound of body weight. The more the better. If you weigh 185 lbs, you should try to get at least 185 grams of protein every day. This amount of protein will help you build muscle and maintain it as you get older. You should try to spread out your protein consumption in roughly equal amounts throughout the day.
- Quote (P. 334): “There’s no minimum requirement for carbohydrates or fats, but if you shortchange protein, you will most certainly pay the price, particularly as you age.”
- Plant Protein vs. Animal Protein — Because protein found in plants is there for the benefit of the plant, it is less effective than protein found in animal sources. The distribution of amino acids is simply not the same as in animal protein. In the end, the overall quality of protein derived from plants is significantly lower than that from animal products. This goes for protein supplements as well; whey protein (from dairy) is richer in amino acids than soy protein.
- Fat — Fat is the third key macronutrient alongside protein and carbs. Fat is essential, but too much of it becomes a problem. While carbs are primarily a source of fuel and protein/amino acids are primarily building blocks, fats are both. They are a very efficient fuel source (think: slow-burning logs) and also the building blocks for many of our hormones (in the form of cholesterol) and cell membranes. Eating the right mix of fats can help maintain metabolic balance, but it is also important for the health of our brain, much of which is composed of fatty acids.
- Types of Fats — There are three main types of dietary fats. The differences between these have to do with differences in their chemical structure; a “saturated” fat simply has more hydrogen atoms attached to its carbon chain. Within PUFA, we make one more important distinction, which is to separate the omega-6 from the omega-3 variants. We further subdivide omega-3 PUFA into marine (EPA, DHA) and nonmarine (ALA) sources. Salmon and other seafood provide the former, nuts and flaxseed the latter. It’s important to remember that virtually no food belongs strictly to one category; food with fat in it usually has a little bit of all three.
- Saturated Fat (SFA) — Try to have saturated fat make up no more than 15-20% of the total fat in your diet.
- Monounsaturated Fat (MUFA) — Try to have MUFA make up no more than 50-55% of the total fat in your diet. Extra virgin olive oil and other vegetable oils are good sources.
- Polyunsaturated Fat (PUFA) — PUFA should then make up the rest of your total fat intake. To help get your PUFA omega-3 EPA and DHA intake, you can eat salmon or take fish oil supplements. These are rich in EPA and DHA.
- Quote (P. 337): “Putting all these changes into practice typically means eating more olive oil and avocados and nuts, cutting back on (but not necessarily eliminating) things like butter and lard, and reducing the omega-6-rich corn, soybean, and sunflower oils — while also looking for ways to increase high-omega-3 marine PUFAs from sources such as salmon and anchovies.”
- Approaching Fat Intake — Our best guess based on the available nutrition studies (which, as discussed previously, aren’t very reliable) is that MUFA is the “best” fat, while PUFA comes in second and has a slight edge over SFA. But the best way to approach fat intake is to find the right mix of fats that work for you, because everybody responds differently. Some people can eat tons of saturated fat and not have any rise in LDL-C or apoB. Others will have big spikes when they eat SFA or any of the other dietary fats. It’s all about monitoring your lipid profile closely so you can get an understanding of how your body responds to the three dietary fats.
- Quote (P. 339): “Subtle changes in fat intake, particularly of saturated fats, can make a significant difference in lipid levels in some people, as I have learned over and over again — but not in others. Some people (like me) can consume saturated fats with near impunity, while others can hardly even look at a slice of bacon without their apoB number jumping to the 90th percentile.”
- Quote (P. 340): “In the final analysis, I tell my patients that on the basis of the least bad, least ambiguous data available, MUFAs are probably the fat that should make up most of our dietary fat mix, which means extra virgin olive oil and high-MUFA vegetable oils. After that, it’s kind of a toss-up, and the actual ratio of SFA and PUFA probably comes down to individual factors such as lipid response and measured inflammation. Finally, unless they are eating a lot of fatty fish, filling their coffers with marine omega-3 PUFA, they almost always need to take EPA and DHA supplements (fish oil) in capsule or oil form.”
- Chapter Takeaway — While nutrition is important, it’s not as important as we’ve been told it is. Exercise is ultimately the best thing we can do for health and longevity. When it comes to nutrition, the key is to make sure you are getting about 1 gram of protein per pound of body weight so you can build and maintain muscle, which is crucial as you get older. Other than that, you should make sure your average glucose levels are staying in a good range by not eating too many simple carb and sugar products. You want to avoid too much saturated fat in your diet as well.
Ch. 16: The Awakening
- Prioritize Sleep — Sleep is critical to your short and long-term health and should be prioritized; 8 hours is ideal, but 9 or 10 is welcome as well. Many studies had found powerful associations between lack of sleep (less than 7 hours, on average) and adverse health effects like metabolic dysfunction, Alzheimer’s, hormonal imbalance, and heart disease. Sleep plays a big role in our day-to-day physical, mental, and emotional wellbeing — we simply feel better in all areas when we sleep well. It’s also very impactful for mental and physical performance.
- Quote (P. 351): “As important as sleep is for the body, it may even be more so for the brain. Good sleep, in terms of not only quantity but quality, is critical to our cognitive function, our memory, and even our emotional equilibrium. We feel better, in every way, after a night of good sleep. Even while we are unconscious, our brain is still working, processing thoughts and memories and emotions (hence, dreams). It even cleans itself, in a manner similar to a city sweeping the streets. Relatedly, there is a growing body of evidence that sleeping well is essential to preserving our cognition as we age and staving off Alzheimer’s disease.”
- Sleep & Performance — Sleep not only affects how we feel, it affects how we perform physically and mentally. Even a single night of bad sleep has been found to have negative consequences on our physical and cognitive performance. Athletes who sleep poorly the night before a race or a match perform markedly worse than when they are well rested. Endurance drops, VO2 Max drops, and one-rep-max strength drops. Several studies, including one focused on the Stanford Men’s Basketball Team, have shown how closely sleep and performance are linked.
- Quote (P. 354): “Good sleep is like a performance-enhancing drug.”
- Sleep & Metabolic Health — Sleep and metabolic health are closely linked. Sleep deprivation, even in the short-term, can cause profound insulin resistance. This isn’t a guess — it’s been proven by at least 9 extensive studies and is one of the most consistent findings in sleep research. Poor sleep can lead to higher levels of insulin in the blood and can hamper your body’s ability to dispose of excess glucose in the bloodstream. Poor sleep can also lead to long-term cardiovascular issues as well.
- Quote (P. 357): “Similar risk associations have been found between poor or short sleep and hypertension (17%), cardiovascular diseases (16%), coronary heart diseases (26%), and obesity (38%). Taken together, these findings all suggest that the long-term effects of inadequate sleep parallel what we would expect from the short-term studies: increased insulin resistance and more of the diseases that accompany it, from NASH and Type 2 diabetes to heart disease. If your sleep is chronically compromised, then your metabolism might be too.”
- Sleep, Stress, and Metabolic Health — Stress is likely the reason sleep and metabolic health are so closely linked. High stress levels can make you sleep poorly, and poor sleep can make you feel more stressed. It’s a loop. Both poor sleep and high stress activate your sympathetic nervous system, which controls your fight-or-flight response and releases the stress hormone cortisol. Cortisol raises blood pressure and prompts the liver to release glucose into the bloodstream. This leads to higher glucose levels — you can easily see it if you have a CGM system and your glucose levels are high overnight. Sleep, stress, and metabolic health are therefore all linked.
- Sleep & Cardiovascular Disease — Stress and poor sleep are closely linked to cardiovascular disease because of the sympathetic nervous system and cortisol response. When you’re not sleeping well and are stressed, your heart rate and blood pressure are up chronically, which puts stress on your arteries. You can tell you’re stressed or are not sleeping well when your heart rate is high overnight and your heart rate variability is low. This can be measured with a heart rate monitor. All of this might explain why inadequate sleep over long periods is associated with increased risk of cardiovascular disease. Sleeping less than six hours has been shown to increase your chances of a heart attack, while sleeping 6-8 hours decreased your chances of a heart attack.
- Quote (P. 359): “Translation: good sleep may help mitigate some of the genetic risk of heart disease faced by people like me. All of the above has convinced me to make sleep a top priority in my own life, and to pay attention to my patients’ sleep habits.”
- Sleep & the Brain — Sleep plays a major role in brain health, especially as you get older, not only in terms of daily cognitive function but also in terms of your long-term cognitive health, which is a crucial pillar of healthspan. Researchers now know that we sleep in a series of well-defined stages, each of which has a specific function and a specific electrical brain wave “signature,” which is how they initially identified the different sleep stages. These stages are:
- Light NREM & Deep NREM — This is the stage where you pass through a period of light sleep before dropping into a deep sleep. Your brain waves are slowing until they reach an extremely low frequency. This deep sleep dominates the first half of the night.
- REM — This is the rapid eye movement (REM) sleep stage. In this state, our eyeballs really will dart around behind our eyelids. We are “seeing” things, but only in our mind. This is where most of our dreaming occurs, as our mind processes images and events that seem familiar but are also strange or dislocated from their typical context. You are in a deep sleep in this stage.
- REM Sleep & Emotions — Interestingly, REM sleep has a way of almost disassociating emotion from memory. For example, if you watch a scary movie at night and then go to bed, any fear you felt the night before will dissolve by the morning with REM sleep. We remember the event but forget the pain that accompanied it. In short, REM sleep seems to protect our emotional equilibrium, while helping us process memories and information.
- Sleep & Cognitive Health — Sleep is not only important when it comes to how your brain functions, it’s important for your overall brain health. Your risk of Alzheimer’s and other neurodegenerative diseases goes up with consistently poor sleep. It’s not enough to be lying in bed — you have to fall into a good sleep for the brain to get the maximum in benefits. Sleep that is irregular, fragmented, or not deep enough will not allow the brain to get all of the benefits.
- Interesting Fact — The drug morphine, a narcotic used to treat pain, was first isolated from the opium poppy in 1806 and was named for Morpheus, the god of dreams, because it put people to sleep quickly and effectively.
- Sleep Medications — For the most part, sleep medications are a bandaid and not a long-term solution. Ambien, Lunesta, Valium, and Xanax do not promote healthy, long-lasting sleep. Instead, they tend to produce a sleep-like state of unconsciousness that doesn’t really accomplish much if any of the brain-healing work of either REM or deep sleep. They knock you out without sending you into a deep, healthy sleep.
- Trazodone & Ashwaganda — Attia has had some success with his patients using trazodone and ashwaganda for sleep. Trazodone is a fairly old anti-depressant (approved in 1981) that never really took off. At the doses used to treat depression, 200-300 milligrams per day, it had the unwanted side effect of causing users to fall asleep.
- Quote (P. 366): “That side effect is what we want in a sleep medication, especially if it also improves sleep architecture, which is exactly what trazodone doe — and most other sleep meds do not. We typically use it at much lower doses, from 100 milligrams down to 50 milligrams or even less; the optimal dosing depends on the individual, but the goal is to find the amount that improves their sleep quality without next-day grogginess.”
- Sleep Tracking — You can use sleep devices to track your heart rate, heart rate variability, breathing patterns, and more. These devices can be very useful in optimizing your sleep and helping you determine how well you are sleeping every night. The key is to avoid going overboard with them. If you get worked up over a bad sleep score, it could cause you to stress out, which leads to more bad sleep. If you tend to get worked up, take a break from the devices.
- Improving Sleep — There are a few notable ways you can create an environment conducive to sleep. Sleep medication is not a long-term answer. Your best bet is to create an environment that gives you to best chance of falling into, and staying in, a deep sleep.
- Eating — Try not to eat inside of three hours before bed. It’s best to go to bed with a little bit of hunger.
- Blue Light — Reduce blue light from your screen/environment wherever possible. Try to stay away from electronics and screens inside of two hours before bed. Blue/unnatural light interferes with your circadian rhythm and blocks the release of melatonin, the darkness-activated hormone that tells your brain it’s time to sleep. Phones, laptops, and TV screens have this blue light.
- Relax — At least one hour before bed, do something that is relaxing and does not involve anything that might induce stress or anxiety. No checking work emails. Watch TV and chill out. Mediate. Anything.
- Shower — A warm shower at night will actually cool your core body temperature, which is what we need to fall asleep.
- Cool Temperature — Cool temperatures are your friend when it comes to sleep. Your body naturally drops in core body temperature when it is falling asleep, so having a cool room and a cool bed helps promote that process. Keep the room at 65 degrees and use a cool mattress/blanket device.
- Darkness — Light, especially blue light, is the enemy at night. Buy blackout shades or invest in a sleep mask.
- Fix Your Wake Time — You should try to get up at the same time every day, even on weekends. This helps you fall into a good circadian rhythm, and trains your body and mind. Your body can almost sense when it’s time to go to sleep and walk-up.
- Insomnia Cruncher — If you deal with insomnia, it can actually help to stay up later to almost force yourself to sleep when you do finally go down to sleep. Going to bed too early for an insomniac can be detrimental. By staying up later, you can help yourself fall asleep. This should only be done to break out of a bad sleep pattern; you ideally want 8 hours of sleep consistently.
- Caffeine — Try to avoid caffeine in the afternoon and evening. Caffeine doesn’t give you energy; it blocks the receptor for a chemical called adenosine, which normally helps us go to sleep every night. Adenosine builds over the course of the day, but consuming caffeine will temporarily block it. The half-life of caffeine in the body is up to 6 hours, so if you drink a cup of coffee at noon you still have a half cup’s worth of caffeine in your system at 6 p.m.
- Chapter Takeaway — Prioritize sleep! The proven benefits of good sleep on metabolic, cognitive, and heart health are too important to ignore. Make sure you’re getting 8 hours of good, quality sleep every night. A big key to getting good sleep is your sleep environment. Make sure yours is conducive to good sleep.
Ch. 17: Work in Progress
- Emotional Health Matters — Your emotional health and well-being are just as important as everything else discussed in this book. Loving yourself and having good relationships with other people are crucial to your overall happiness in life. Your emotional health has to be worked on every day.
- Reframing & Empathy — One of the great ways to cool down and not get overly mad or frustrated in life is to reframe the situation. Take a step back and try to see things from the other person’s perspective.
- Eulogy Virtues vs Resume Virtues — It’s very easy to get caught up chasing work goals and achievements (things that add to your resume), but your focus should never stray away from building ‘eulogy virtues’, which are more about making an impact on people’s lives. How will people talk about you at your funeral? At the end of the day, you want to help people and make a difference. Do small things that make somebody’s day. Do big things that can change a person’s life. This should always be one of your top priorities in life.
- Quote (P. 410): “Your résumé doesn’t really matter, either, when it comes time for your eulogy. All these need to be addressed if your life is to be worth prolonging — because the most important ingredient in the whole longevity equation is the why. Why do you want to live longer? For what? For whom?”
- Mindfulness & Self-Talk — Practicing mediation and mindfulness is a great way to get out of your negative thoughts and stay in the moment. When it comes to self-talk, the key is to be kind to yourself. It’s easy to be tough on yourself; that’s our natural reaction. When you mess up, don’t beat yourself up — encourage yourself like you would a close friend. Be your own No. 1 fan.
- Cold & Deep Breathing — Splashing cold water on your face or getting into a cold shower or ice bath can help induce an abrupt sensory change that calms you down. Deep breathing is also extremely beneficial and should be practiced often. With practice, you can begin to control your nervous system with your breath.
- Quote (P. 404): “One simple tactic that I use to cope with mounting emotional distress is inducing an abrupt sensory change — typically, by throwing ice water on my face or, if I’m really struggling, taking a cold shower or stepping into an ice bath. This simple intervention stimulates an important cranial nerve, the vagus nerve, which causes our heart rate and respiratory rate to slow and switches us into a calm, parasympathetic mode (and out of our fight-or-flight sympathetic mode).”
- Quote (P. 405): “Another technique I have grown very fond of is slow, deep breathing: four seconds to inhale, six seconds to exhale. Repeat. As the breath goes, the nervous system follows.”